Master Behavioral Health Electronic Medical Records Software for Success

Introduction
Behavioral health electronic medical records (EMRs) are fundamentally reshaping the mental health care landscape. They present significant opportunities for enhancing patient outcomes and operational efficiency. By centralizing essential patient information, these systems streamline documentation, improve communication among care teams, and ensure compliance with regulatory standards.
However, the adoption of this technology is not without its challenges. Organizations often encounter staff resistance and integration hurdles that can impede progress. To fully harness the potential of EMRs in behavioral health settings, it is crucial to identify and implement effective strategies to overcome these obstacles.
Understand the Importance of Behavioral Health EMRs
Behavioral health electronic medical records software is crucial in modern healthcare, particularly for managing individual data within behavioral health settings. Behavioral health electronic medical records software not only streamlines documentation but also enhances communication among care teams and ensures compliance with regulatory standards. By centralizing individual information, behavioral health electronic medical records software significantly enhances decision-making and outcomes for individuals.
For example, behavioral health electronic medical records software offers real-time access to patient histories, treatment plans, and progress notes, which are vital for effective care coordination. Additionally, behavioral health electronic medical records software simplifies billing processes and helps organizations adhere to the stringent standards set by medical regulations. This ultimately leads to improved operational efficiency and reduced administrative challenges.

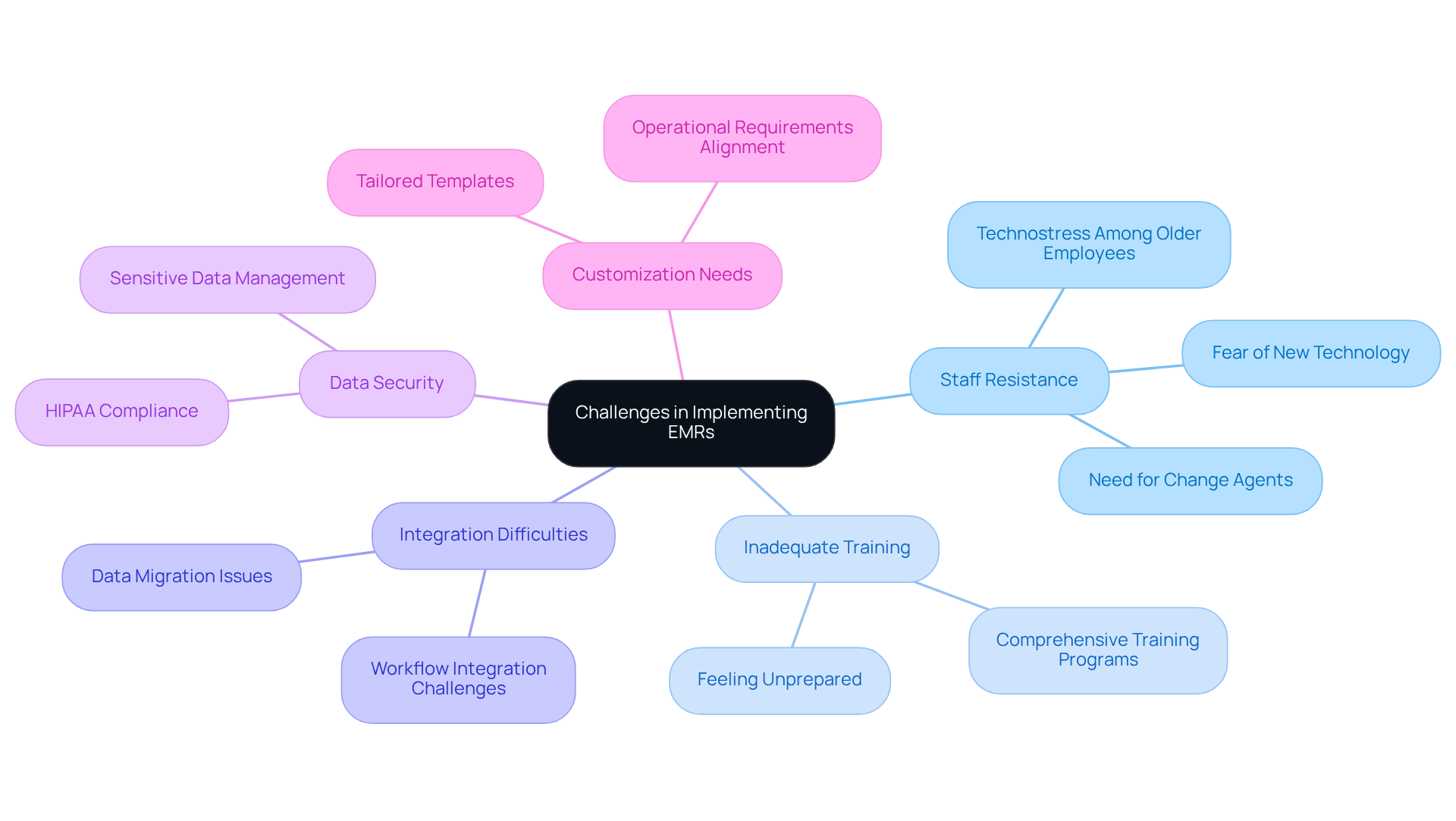
Identify Challenges in Implementing EMRs
Implementing behavioral health electronic medical records software presents significant challenges that organizations must navigate effectively. A primary hurdle is staff resistance to change, often stemming from a lack of understanding or fear of new technology. Research indicates that a substantial portion of healthcare staff experiences technostress, particularly among older employees who may find it more difficult to adapt to EMR systems. This resistance can lead to decreased engagement and underutilization of the EMR, ultimately impacting patient care. By 2021, 96% of hospitals had adopted certified EHRs, underscoring the widespread transition to electronic medical records and the associated challenges, particularly regarding staff resistance and training.
Inadequate training exacerbates these issues, as staff may feel unprepared to use the new system effectively. Organizations frequently encounter difficulties in integrating electronic medical records with existing workflows, which can impede the transition process. Additionally, maintaining data security and adhering to HIPAA regulations remains a challenging endeavor, particularly due to the sensitive nature of behavioral wellness data. As of 2023, 71% of hospitals had routine access to external clinical information, highlighting the importance of data integration and its impact on EMR effectiveness.
The personalization of behavioral health electronic medical records software to address specific behavioral wellness needs is another crucial factor. For instance, Cherokee Health developed its own behavioral health electronic medical records software with tailored templates to meet their operational requirements, demonstrating how customized solutions can address implementation challenges. Without such customization, organizations risk implementing systems that do not fully support their operational needs, leading to frustration and disengagement among staff.
To mitigate these challenges, engaging stakeholders early in the implementation process is essential. Providing comprehensive training and fostering a culture of openness can significantly reduce resistance. As noted by Diana Altynbaeva, overcoming staff resistance is crucial for successful implementation. Successful organizations often create change agent teams to facilitate communication and address concerns, ensuring that the chosen EMR system aligns with the organization’s workflows and goals. By prioritizing these strategies, medical providers can enhance the likelihood of a successful EMR implementation, ultimately improving patient outcomes and operational efficiency.
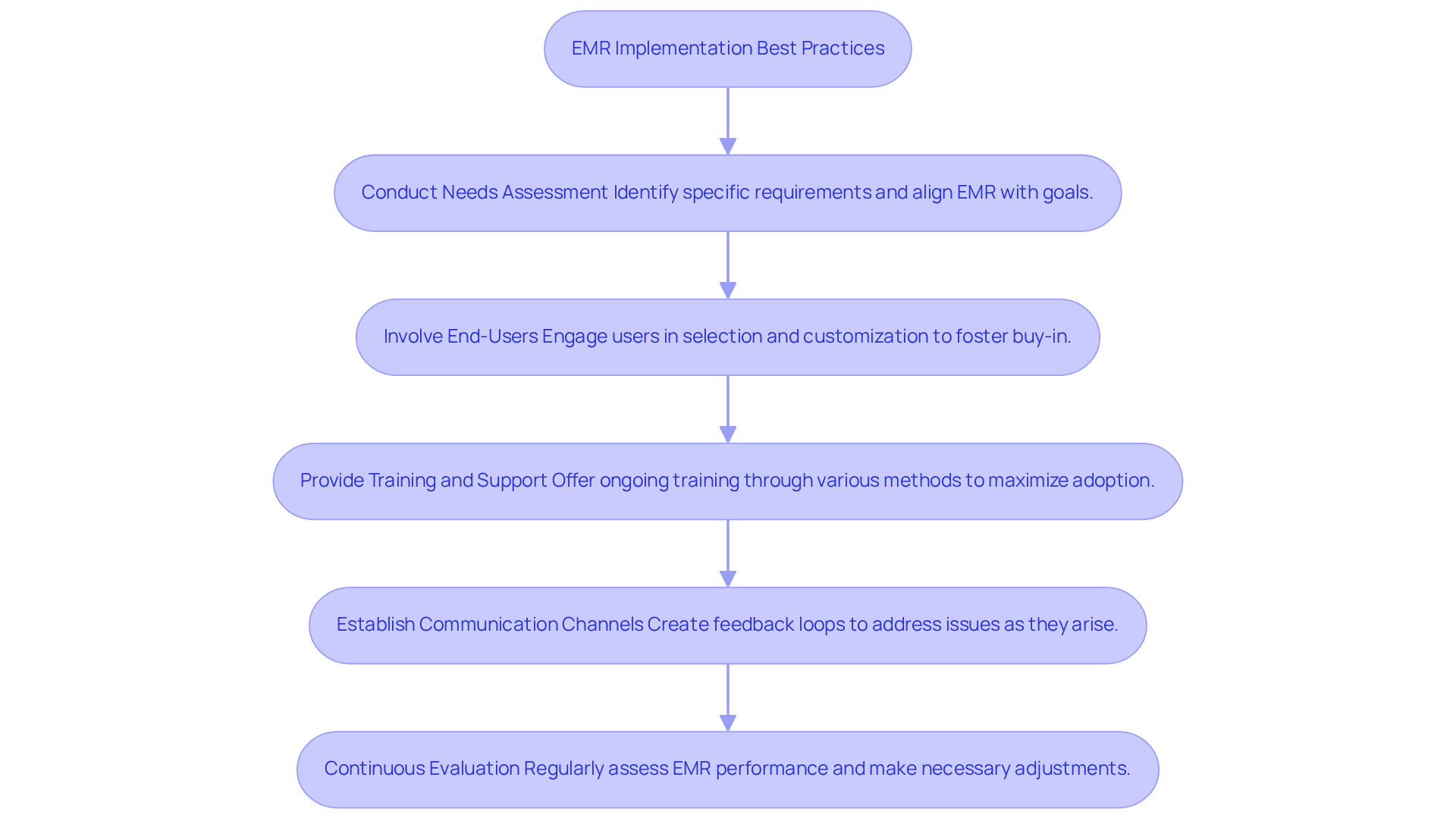
Adopt Best Practices for EMR Implementation
To successfully implement Behavioral Health EMRs, organizations should adopt several best practices. Conducting a thorough needs assessment is essential; it helps identify specific requirements and ensures the selected EMR aligns with organizational goals. This process should involve key stakeholders, including medical providers and IT personnel, to gather diverse insights and foster a collaborative environment. As Stacey LaCotti notes, “The adoption of electronic health records is essential to contemporary healthcare delivery because it directly impacts accuracy, efficiency, and outcomes for individuals.”
Involving end-users in the selection and customization process of behavioral health electronic medical records software is another critical step. This approach fosters buy-in and reduces resistance to the new system. Furthermore, providing ongoing training and support is crucial for maximizing user adoption and proficiency. Training methods should encompass in-person sessions, online courses, and hands-on experience to cater to different learning preferences.
Additionally, establishing clear communication channels and feedback loops can help address issues as they arise. Statistics indicate that 93% of hospitals have adopted certified EHR systems, underscoring the importance of robust training and support during implementation.
Finally, organizations should continuously evaluate the EMR’s performance and make necessary adjustments to optimize its use. It is also vital to be mindful of common pitfalls, such as provider burden and technostress, which can hinder successful adoption.
Explore Future Innovations in EMR Technology
The future of behavioral health electronic medical records software is set to undergo significant transformations driven by advancements in technology. At the forefront of this evolution are artificial intelligence (AI) and machine learning, which are markedly enhancing data analysis capabilities. These technologies facilitate predictive analytics, allowing for the forecasting of individual outcomes and the tailoring of personalized treatment plans, ultimately leading to improved quality of care. Notably, there are 32 emerging trends and technology themes shaping generative AI in HealthTech and MedTech markets, highlighting the importance of these developments.
Moreover, the integration of telehealth functionalities within behavioral health electronic medical records software is revolutionizing patient engagement. By enabling remote monitoring and virtual consultations, these advancements broaden access to essential services. A pertinent example is CalOptima Health, which has successfully implemented accessible mental health services that demonstrate the practical application of these technologies.
Additionally, blockchain technology is emerging as a vital component, enhancing data security and ensuring interoperability across diverse medical systems. As organizations navigate these innovations, it is imperative to stay informed about these trends and strategically leverage new technologies, including behavioral health electronic medical records software, to optimize EMR systems and elevate overall patient care. However, awareness of potential pitfalls in the integration of these technologies, such as fragmented data infrastructure and regulatory complexities, is crucial.
By embracing these advancements, healthcare providers can enhance operational efficiency while fostering a more responsive and patient-centered approach to behavioral well-being. Industry leaders note that the trajectory of care delivery is shifting towards more connected behavioral health ecosystems, integrating both in-person and virtual offerings, augmented by AI-guided mental health support.

Conclusion
Behavioral health electronic medical records (EMRs) play a crucial role in improving the quality of care within mental health settings. By streamlining documentation, enhancing communication among care teams, and ensuring compliance with regulations, these systems enable healthcare providers to offer more effective and personalized treatment. The successful implementation of behavioral health EMRs can lead to notable improvements in operational efficiency and patient outcomes, making it essential for organizations to adopt this technology.
This article has highlighted several key aspects of behavioral health EMRs. Understanding the challenges associated with their implementation – such as staff resistance and the necessity for adequate training – is vital. Organizations must prioritize stakeholder engagement and adopt best practices to effectively navigate these challenges. Additionally, exploring future innovations, including AI and telehealth integration, underscores the ongoing evolution of EMR technology and its potential to transform patient care.
As the landscape of behavioral health continues to change, it is imperative for healthcare providers to proactively adopt and optimize EMR systems. By leveraging the insights and strategies discussed, organizations can enhance their operational efficiency while fostering a more responsive and patient-centered approach to care. Embracing these advancements is not merely about keeping pace with technology; it is about ensuring that every individual receives the highest level of support for their mental health needs.
Frequently Asked Questions
What is the role of behavioral health electronic medical records (EMRs) in healthcare?
Behavioral health EMRs are crucial for managing individual data in behavioral health settings, streamlining documentation, enhancing communication among care teams, and ensuring compliance with regulatory standards.
How do behavioral health EMRs improve decision-making and outcomes?
By centralizing individual information, behavioral health EMRs provide real-time access to patient histories, treatment plans, and progress notes, which are essential for effective care coordination and improved decision-making.
What are some benefits of using behavioral health EMRs?
Benefits include simplified billing processes, adherence to medical regulations, improved operational efficiency, and reduced administrative challenges.
How do behavioral health EMRs enhance communication among care teams?
Behavioral health EMRs facilitate better communication by providing centralized access to important patient information, which helps care teams coordinate more effectively.
In what ways do behavioral health EMRs ensure compliance with regulatory standards?
They help organizations adhere to stringent standards set by medical regulations by maintaining accurate and organized documentation of patient data.