Maximize Efficiency with Physician Practice Management Software

Introduction
Physician practice management software (PMS) has emerged as a pivotal solution for healthcare facilities, addressing the pressing need for operational efficiency in an increasingly complex medical landscape. By automating essential tasks such as appointment scheduling, billing, and client records management, PMS streamlines workflows and enhances patient care and satisfaction.
However, as organizations seek to maximize the benefits of these systems, they often face challenges related to integration and staff training. Thus, medical practices must navigate these hurdles to fully leverage the capabilities of physician practice management software.
Understand Core Functions of Physician Practice Management Software
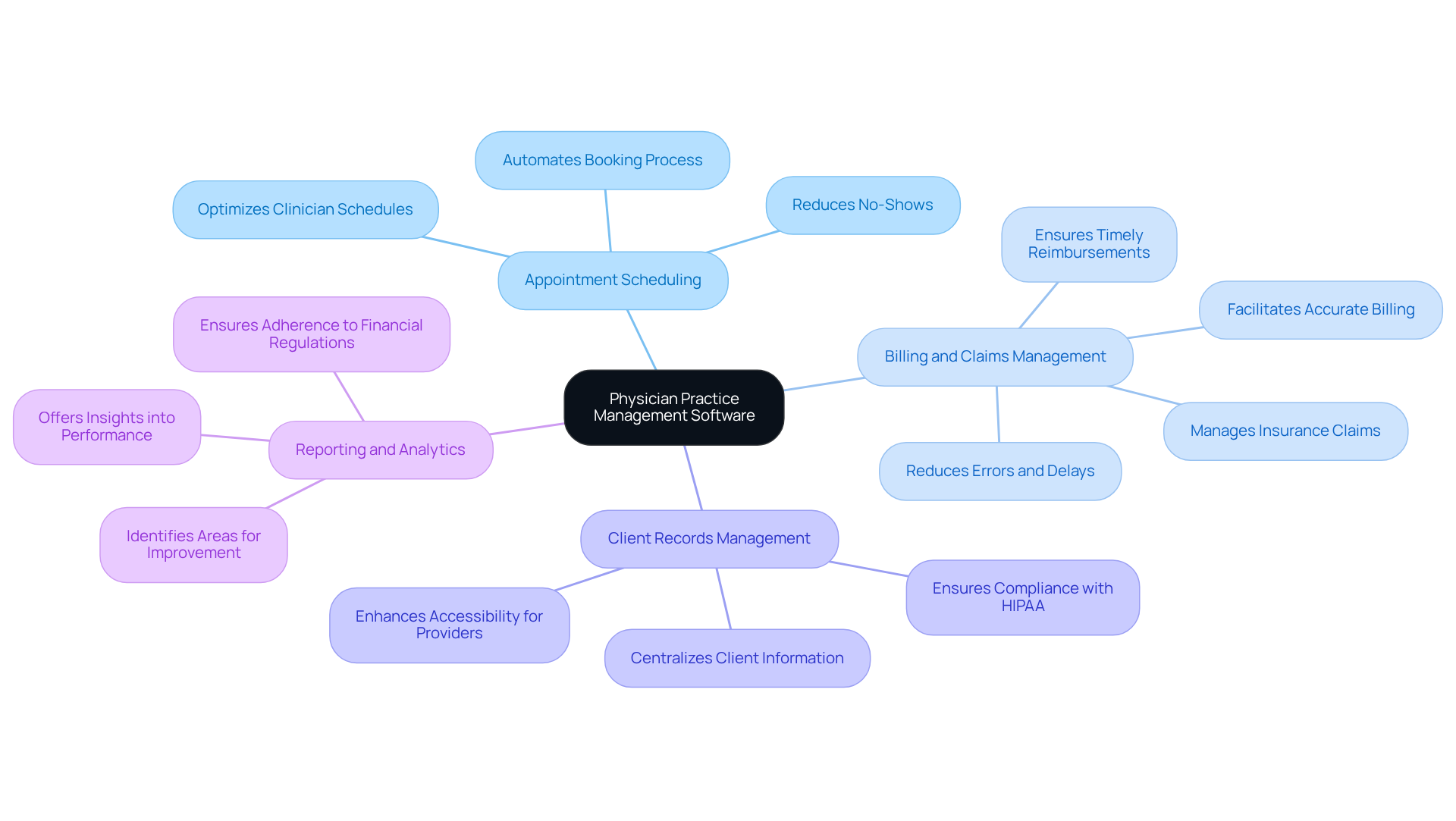
Physician practice management software (PMS) serves as a comprehensive tool designed to streamline various administrative tasks within medical facilities. Its key functions include:
-
Appointment Scheduling: This feature automates the booking process, effectively reducing no-shows and optimizing clinician schedules. According to Black Book Market Research, practices are increasingly prioritizing day-to-day operational efficiency, which encompasses workflow practicality and minimized administrative tasks. This underscores the importance of effective scheduling systems.
-
Billing and Claims Management: PMS facilitates accurate billing processes and manages insurance claims, ensuring timely reimbursements. The automation of billing reduces errors and delays, thereby contributing to consistent revenue growth.
-
Client Records Management: This function centralizes client information, making it readily accessible for healthcare providers while ensuring compliance with regulations such as HIPAA. Such accessibility is crucial for maintaining high standards of care for individuals.
-
Reporting and Analytics: PMS offers insights into operational performance, aiding in the identification of areas for improvement and ensuring adherence to financial regulations. By leveraging data analytics, organizations can enhance operational outcomes and client engagement.
Additionally, the case study ‘The First Appointment Advantage: How Trust is Earned Before the Exam Room’ emphasizes the importance of establishing trust with individuals through efficient appointment scheduling. This can significantly enhance satisfaction and lead to improved health outcomes. Understanding these essential functions enables medical facilities to utilize physician practice management software effectively, which ultimately enhances patient care and operational efficiency.
Identify Key Features for Enhanced Operational Efficiency
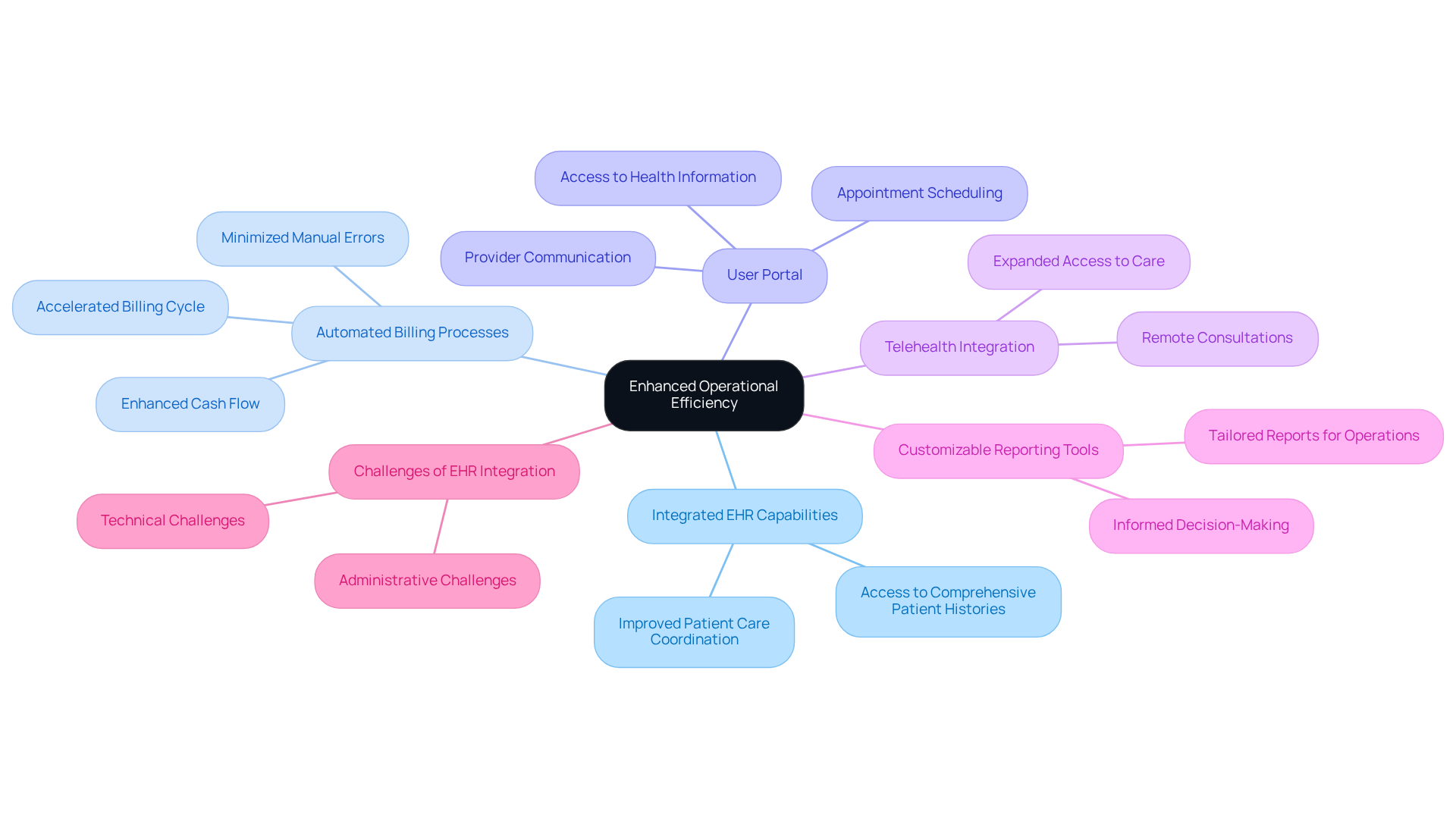
When selecting physician practice management software, prioritizing features that enhance operational efficiency is essential. Among these, integrated EHR capabilities emerge as a cornerstone for effective medical delivery. Seamless integration with Electronic Health Records (EHR) systems facilitates superior data management and enhances patient care coordination, enabling healthcare providers to access comprehensive patient histories at the point of care.
Automated billing processes within physician practice management software further streamline operations by minimizing manual errors and accelerating the billing cycle, significantly enhancing cash flow for businesses. For instance, NexHealth assists practices in saving hundreds of hours on monthly labor through automation, reinforcing the efficiency benefits of integrated EHR capabilities. Additionally, a user portal allows individuals to access their health information, schedule appointments, and communicate with providers, thereby promoting greater engagement and satisfaction.
Telehealth integration is an essential feature of physician practice management software, enabling remote consultations that expand access to care and enhance patient experiences. CareCloud Charts provide real-time intelligence at the point of care to support critical decision-making, underscoring the advantages of integrated EHR systems. Lastly, customizable reporting tools empower practices to generate tailored reports that address specific operational and financial needs, driving informed decision-making.
While these features collectively streamline workflows and contribute to improved patient outcomes and satisfaction, it is important to acknowledge the challenges associated with achieving full EHR integration. As noted by IT specialists in the medical field, integration presents technical and administrative challenges that require organizations to align around standards and processes. Addressing these challenges is crucial for maximizing the benefits of integrated EHR capabilities in medical software.
Leverage Integration for Streamlined Workflows
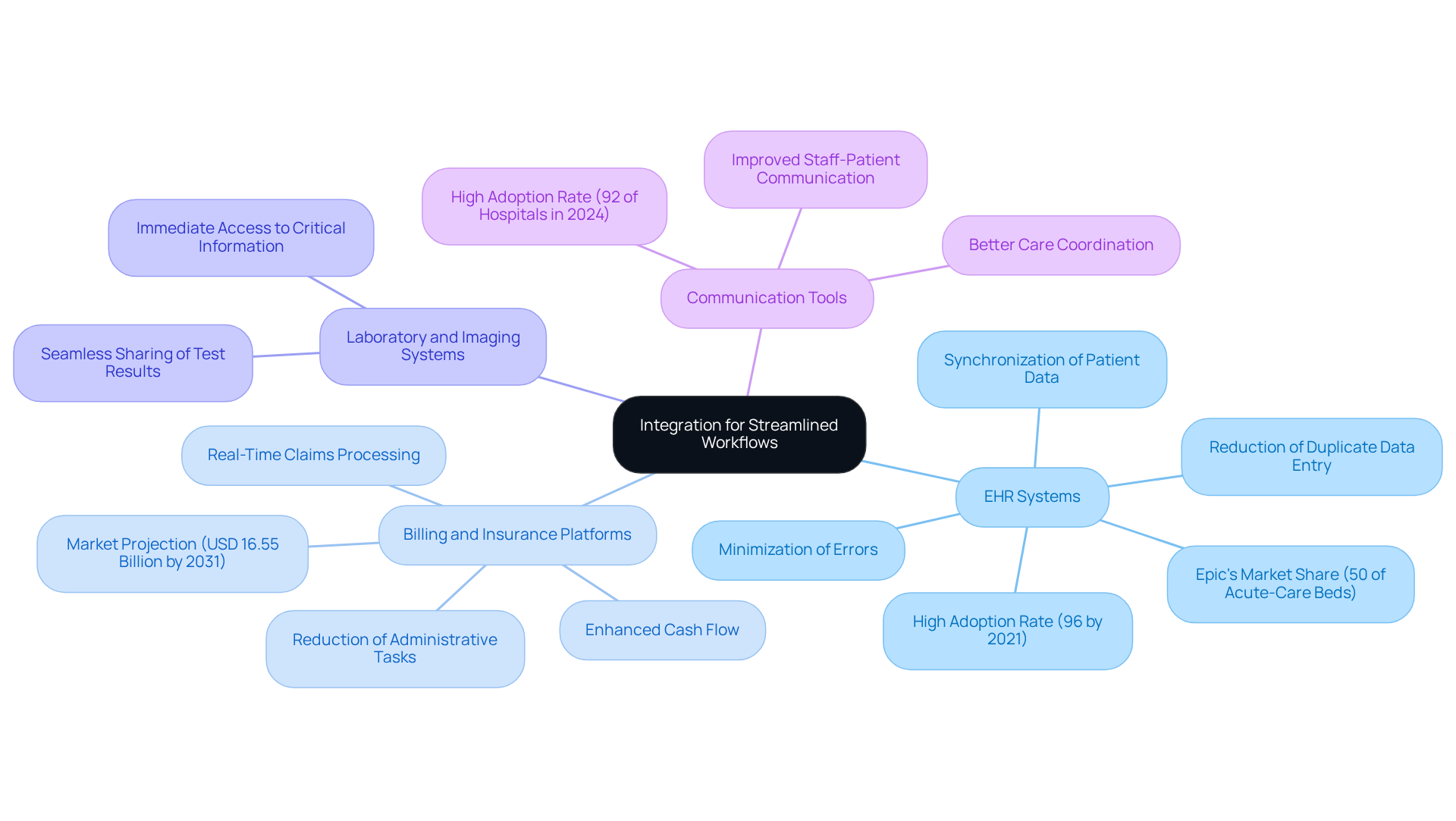
Integrating physician practice management software with healthcare networks is crucial for streamlining workflows and enhancing operational efficiency. Key integration points include:
-
EHR Systems: Connecting PMS with electronic health record (EHR) systems ensures synchronization of patient data, significantly reducing duplicate data entry and minimizing errors. This integration is vital, as 96% of hospitals had adopted certified EHRs by 2021, highlighting the reliance on these solutions. Furthermore, with Epic managing over 50% of acute-care multispecialty beds in the U.S. as of 2024, the significance of EHR platforms in the healthcare landscape is undeniable.
-
Billing and Insurance Platforms: Integrating with billing systems allows for real-time claims processing and tracking, essential for effective revenue cycle management. This capability streamlines billing processes, ultimately enhancing cash flow and reducing the time spent on administrative tasks. The physician practice management software market is projected to reach USD 16.55 billion by 2031, underscoring the increasing importance of these integrations.
-
Laboratory and Imaging Systems: Linking laboratory and imaging systems with PMS facilitates the seamless sharing of test results and imaging reports directly within the practice management interface. This integration enhances clinical decision-making by providing healthcare providers with immediate access to critical information about patients.
-
Communication Tools: Incorporating secure messaging platforms into PMS improves communication between staff and patients, leading to better care coordination. With 92% of hospitals enabling secure messaging with providers in 2024, this feature is becoming increasingly vital for fostering patient engagement and satisfaction.
Despite these advantages, challenges such as increased administrative burden and workflow disruptions related to EHR adoption persist. Addressing these issues is essential for maximizing the benefits of integration. By leveraging these integrations, healthcare organizations can significantly reduce administrative overhead, enhance revenue cycle management, and improve overall operational efficiency.
Implement Training and Support for Staff Proficiency
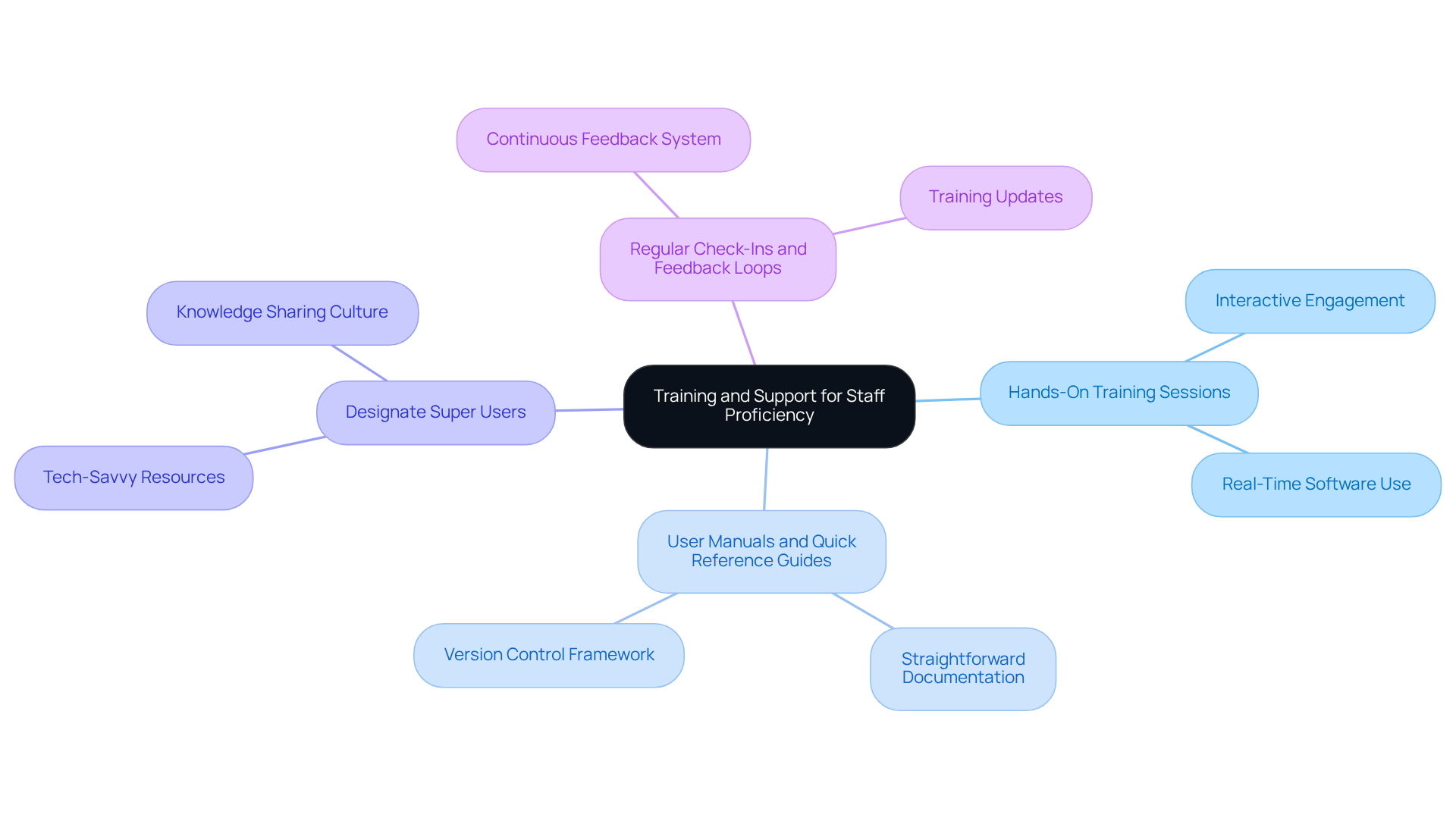
To fully leverage the advantages of physician practice management software, implementing a robust training and support framework for staff is essential. Key strategies include:
- Hands-On Training Sessions: Facilitate interactive training sessions that allow staff to engage with the software in real-time, significantly boosting their comfort and proficiency levels. As noted, “User guides and QRGs accommodate various learning preferences, ensuring that all staff possess the essential resources to excel in utilizing the EPR platform.”
- Create User Manuals and Quick Reference Guides: Develop straightforward documentation that staff can easily consult while using the software, thereby minimizing dependence on IT support. A robust version control framework is crucial for managing updates to these guides, ensuring staff refer to current information and reducing confusion.
- Designate Super Users: Identify tech-savvy team members to act as primary resources for their colleagues, promoting a culture of support and knowledge sharing within the practice. This approach aligns with findings that “user guides and QRGs help reinforce knowledge and skills gained during training sessions.”
- Regular Check-Ins and Feedback Loops: Implement a system for continuous feedback and training updates to address any challenges staff encounter and to keep them informed about new features. Ongoing support is critical for maintaining proficiency, as highlighted in the key points regarding the importance of user training.
Investing in these training and support initiatives ensures that staff become proficient in utilizing the physician practice management software, ultimately leading to enhanced operational efficiency and improved patient care. Knowledge transfer and user training typically take 2-5 weeks, setting clear expectations for the training process.
Conclusion
Maximizing efficiency within healthcare practices is essential for delivering high-quality patient care and maintaining operational effectiveness. Physician practice management software is a crucial tool in this endeavor, offering functionalities that streamline administrative tasks, enhance communication, and improve overall workflow. By leveraging these systems, medical facilities can significantly boost productivity and patient satisfaction.
The article highlights several key features of physician practice management software, including:
- Appointment scheduling
- Billing and claims management
- Client records management
- Reporting capabilities
Each function plays a vital role in ensuring that healthcare providers operate smoothly and can focus on patient care. Furthermore, the integration of EHR systems and other platforms facilitates seamless data sharing, further enhancing operational efficiency.
Given the critical importance of these software solutions, healthcare organizations are encouraged to invest in comprehensive training and support for their staff. By prioritizing user proficiency and fostering a culture of continuous learning, practices can fully harness the potential of physician practice management software. Embracing these best practices not only improves operational efficiency but also leads to better patient outcomes, reinforcing the value of adopting such technologies in the healthcare landscape.
Frequently Asked Questions
What is physician practice management software (PMS)?
Physician practice management software (PMS) is a comprehensive tool designed to streamline various administrative tasks within medical facilities, enhancing operational efficiency and patient care.
What are the key functions of PMS?
The key functions of PMS include appointment scheduling, billing and claims management, client records management, and reporting and analytics.
How does appointment scheduling work in PMS?
The appointment scheduling feature automates the booking process, reducing no-shows and optimizing clinician schedules, which is essential for improving day-to-day operational efficiency.
What role does PMS play in billing and claims management?
PMS facilitates accurate billing processes and manages insurance claims, ensuring timely reimbursements and reducing errors and delays, which contributes to consistent revenue growth.
How does PMS manage client records?
PMS centralizes client information, making it easily accessible for healthcare providers while ensuring compliance with regulations such as HIPAA, which is crucial for maintaining high standards of care.
What benefits does reporting and analytics provide in PMS?
Reporting and analytics in PMS offer insights into operational performance, helping identify areas for improvement and ensuring adherence to financial regulations, thus enhancing operational outcomes and client engagement.
How does efficient appointment scheduling impact patient care?
Efficient appointment scheduling helps establish trust with individuals, which can significantly enhance patient satisfaction and lead to improved health outcomes, as highlighted in the case study ‘The First Appointment Advantage: How Trust is Earned Before the Exam Room.