10 Revenue Cycle Management Software Vendors to Consider

Introduction
In the dynamic realm of healthcare, the efficiency of revenue cycle management (RCM) has emerged as a pivotal concern for medical organizations aiming to enhance their financial stability. With an estimated annual loss of $262 billion attributed to denied medical claims, the necessity for effective RCM software solutions has never been more urgent.
This article explores ten distinguished vendors that provide innovative and customized RCM solutions, illustrating how their distinct methodologies can assist healthcare providers in navigating the intricacies of billing, improving operational efficiency, and ultimately bolstering their financial performance.
As the industry confronts escalating challenges, which of these vendors will prove to be the key to achieving financial success?
Neutech: Tailored Revenue Cycle Management Solutions for Healthcare
Neutech stands out among revenue cycle management software vendors by delivering tailored RCM solutions that address the unique challenges faced by regulated industries. By emphasizing compliance and operational efficiency, Neutech empowers medical providers to adeptly navigate the complex billing and coding landscape. The firm’s engineers, who have undergone rigorous training through a demanding residency program, bring senior-level expertise, enabling medical organizations to optimize their revenue potential.
The reliability of Neutech is reflected in its impressive employee retention rate, which guarantees that clients benefit from a stable and knowledgeable team. Furthermore, Neutech’s zero-bench philosophy ensures that every engineer is actively engaged, promoting seamless scalability and consistent quality in service delivery. This strategic approach not only enhances operational efficiency but also positions organizations to improve their financial performance in an increasingly competitive environment.
With 5% to 10% of medical claims denied each year, translating to a potential loss of up to $262 billion for the industry, the need for effective solutions from revenue cycle management software vendors is paramount. Neutech’s customized systems, developed by revenue cycle management software vendors, can reduce claim denial rates by as much as 75%, significantly bolstering overall economic health.
Additionally, Neutech’s client engagement process includes personalized consultations and a careful selection of specialized developers and designers, ensuring that the unique needs of each medical provider are met. Monitoring and optimizing key performance indicators (KPIs) is crucial for assessing economic performance, further highlighting the value of Neutech’s RCM solutions.

NextGen Healthcare: Integrated Revenue Cycle Management and EHR Solutions
NextGen Healthcare provides a comprehensive integrated solution for revenue cycle management software vendors and electronic health records (EHR) that significantly enhances billing processes and overall financial performance for medical practitioners. By merging RCM with EHR functionalities, NextGen empowers medical organizations to manage client data and billing seamlessly, thereby minimizing errors and accelerating collections. This platform is tailored to meet the diverse requirements of various medical practices, allowing providers to concentrate on delivering high-quality patient care while maintaining robust financial health.
As of 2026, NextGen Healthcare is a market leader, holding a substantial share in financial cycle management, which reflects its dedication to innovation and efficiency in medical services. Success stories from providers utilizing revenue cycle management software vendors, like NextGen’s RCM solutions, reveal notable enhancements in cash flow and decreased denial rates, highlighting the effectiveness of their integrated approach. As the medical landscape continues to evolve, NextGen remains at the forefront, adapting its solutions to address the challenges posed by rising costs and complex payer environments.
Athenahealth: Cloud-Based Revenue Cycle Management for Enhanced Billing Efficiency
Athenahealth provides a cloud-based financial cycle management solution that significantly enhances billing efficiency for medical providers. By utilizing cloud technology, Athenahealth enables real-time access to billing data, which facilitates faster claim submissions and improved tracking of reimbursements. The platform is specifically designed to reduce administrative burdens, allowing medical professionals to focus more on patient care while ensuring that financial processes are streamlined and effective.
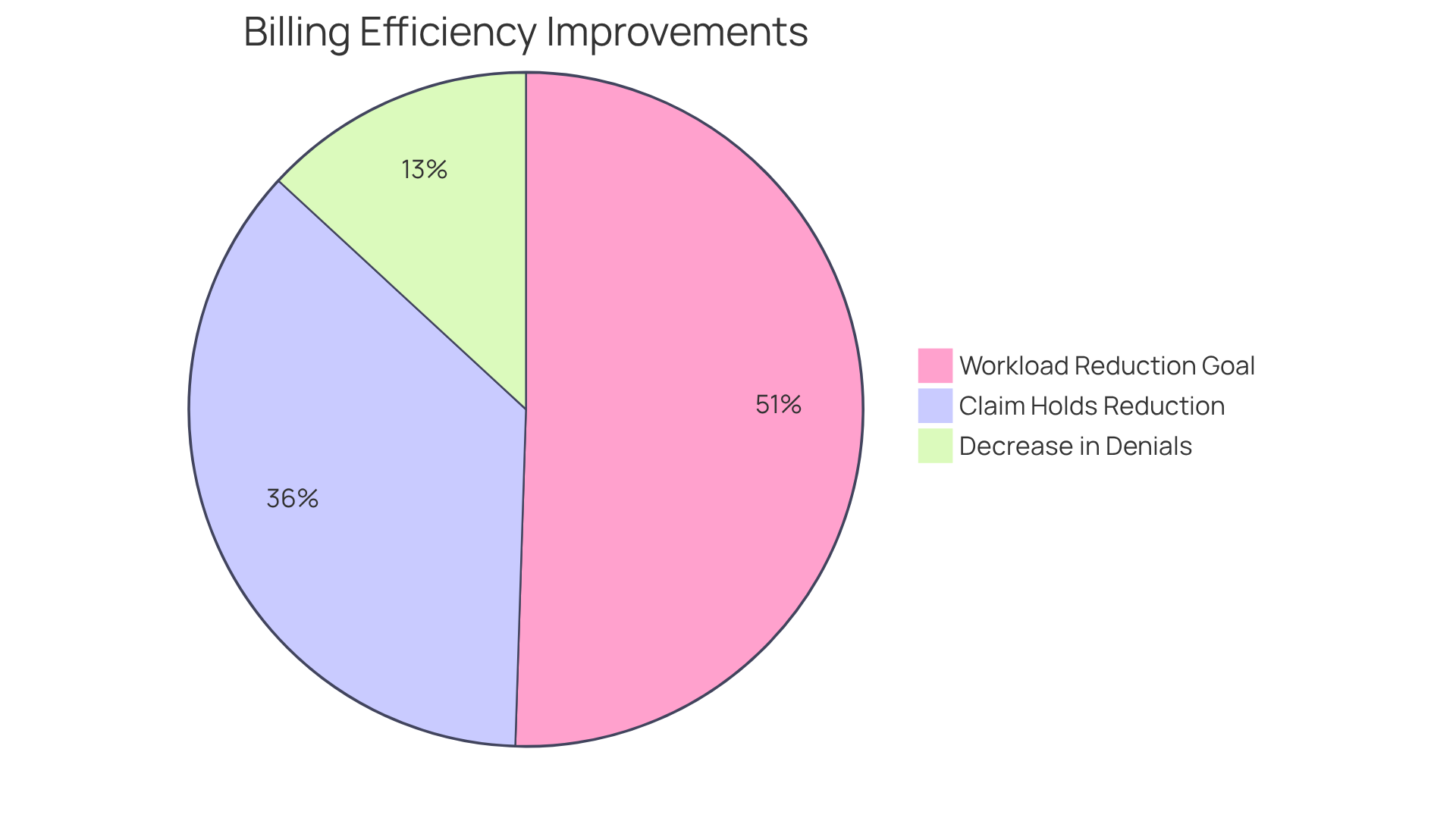
In 2025, Athenahealth introduced AI-enabled features that have already resulted in a 36% reduction in insurance-related claim holds, translating to over 6,500 hours saved in administrative time. With the goal of reducing at least 50% of the current financial cycle management workload over the next three years, Athenahealth is poised to transform how providers manage their billing processes. Paul Brient, chief product officer at Athenahealth, remarked, “Athenahealth’s innovations are designed to dramatically reduce the administrative complexity that burdens practices and improve outcomes for revenue cycle management software vendors.”
Healthcare providers utilizing solutions from revenue cycle management software vendors such as Athenahealth have reported notable improvements in billing efficiency, underscoring the platform’s capability to enhance operational workflows. The integration of cloud technology not only accelerates reimbursements but also assists medical organizations in navigating the complexities of evolving health policies. Furthermore, the automated insurance selection feature decreases patient insurance-related denials by 13%, further demonstrating the effectiveness of Athenahealth’s solutions in enhancing billing efficiency. As the medical landscape continues to evolve, Athenahealth’s commitment to innovation positions it as a leader in improving billing efficiency for medical practices.
Cerner: Optimizing Financial Performance with Revenue Cycle Management Tools
Cerner provides a comprehensive suite of financial cycle management tools designed to significantly enhance the fiscal performance of medical organizations. By automating critical processes such as claims submission and eligibility verification, Cerner effectively reduces claim denials and accelerates income capture. Medical organizations that have adopted Cerner’s solutions report a marked decrease in claim denials, which is vital for sustaining cash flow and operational efficiency. Furthermore, cash collections can increase by as much as 48% when financial cycle management is outsourced and automated, underscoring the effectiveness of Cerner’s offerings.
The automation capabilities of Cerner’s tools not only streamline workflows but also ensure compliance with industry regulations, enabling providers to concentrate on delivering high-quality care. As healthcare organizations face escalating operational costs and complex reimbursement frameworks, enhancing financial cycle management becomes essential for economic sustainability. By 2026, the emphasis on automation is expected to grow, with many organizations prioritizing investments in AI-driven analytics to further refine their financial cycle operations.
Financial experts emphasize that minimizing claim denials is a critical strategy for improving overall financial performance. As one specialist noted, “Minimizing claim denials is crucial for maximizing revenue and ensuring economic health in today’s competitive environment.” With Cerner’s advanced automation capabilities, providers can anticipate a significant positive impact on their economic well-being, positioning them to thrive in an increasingly competitive landscape. Additionally, addressing rising cybersecurity challenges through automation will bolster the security of financial operations and enhance patient trust.
McKesson: Cost-Effective Revenue Cycle Management Solutions
McKesson provides solutions through revenue cycle management software vendors that are both affordable and effective, enabling medical providers to enhance their financial operations. This platform is specifically designed to reduce operational costs while maximizing revenue through streamlined billing processes and improved claims management.
By delivering adaptable and customized solutions that cater to the unique needs of medical organizations, McKesson empowers clients to achieve economic sustainability without sacrificing service quality. This approach not only enhances operational efficiency but also supports the long-term financial stability of medical facilities, allowing them to focus on delivering exceptional patient care.
eClinicalWorks: Innovative Revenue Cycle Management for Healthcare Providers
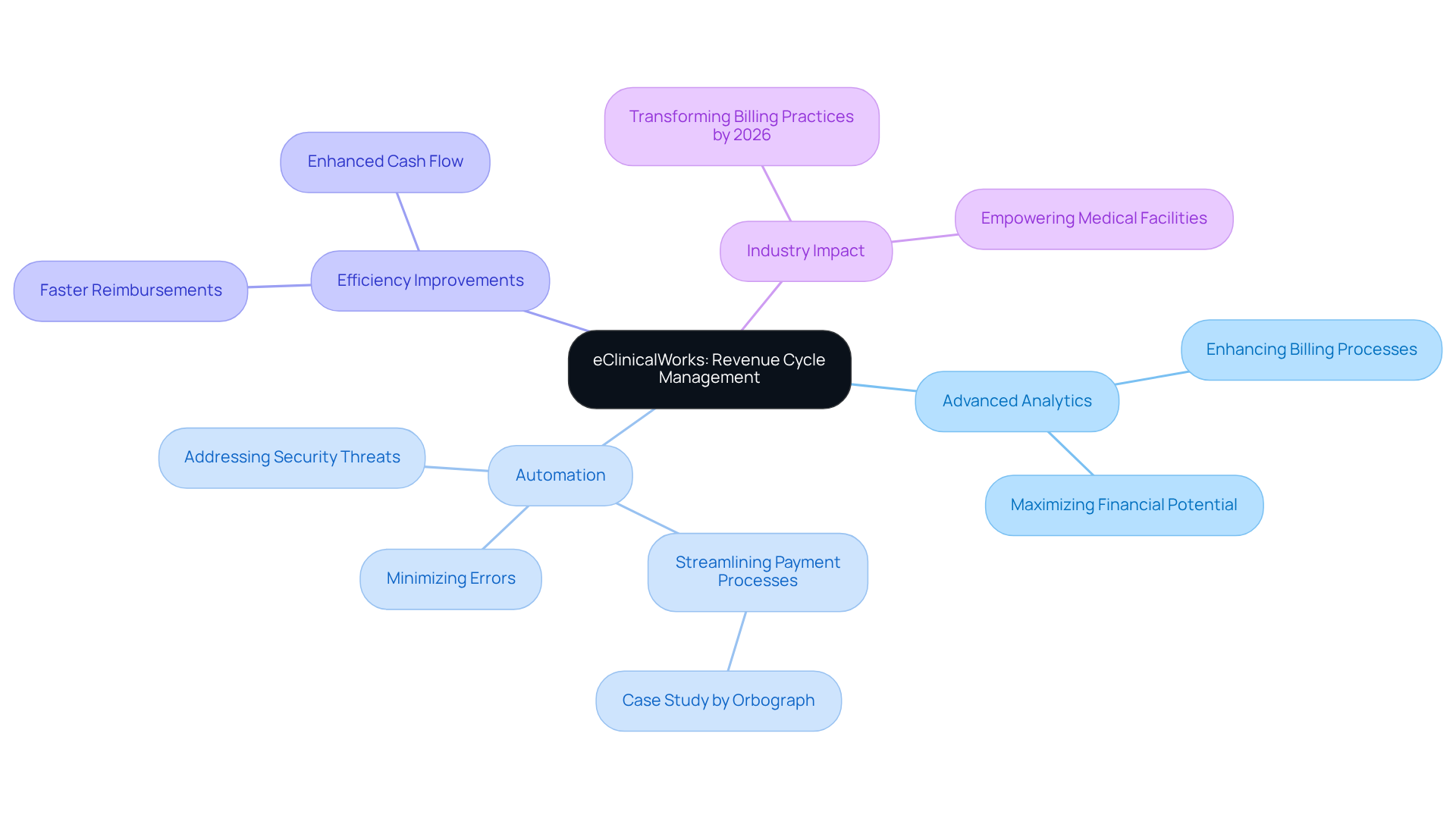
eClinicalWorks distinguishes itself among revenue cycle management software vendors through its advanced cycle management solutions tailored for medical providers. This platform utilizes advanced analytics and automation to enhance billing processes, significantly minimizing errors and boosting financial performance. By 2026, the integration of these technologies is expected to transform billing practices, enabling medical organizations to respond adeptly to evolving market demands while ensuring compliance and maximizing financial potential.
For example, medical providers using eClinicalWorks have reported improved efficiency in their revenue cycle management software vendors, resulting in faster reimbursements and enhanced cash flow. A case study by Orbograph highlights that their P2Post and E2Post services have automated the posting of receivables, streamlining payment processes for medical organizations. Experts in medical analytics assert that automation is vital for optimizing billing processes, allowing organizations to concentrate on patient care rather than administrative tasks. Furthermore, as noted by Emind, leveraging automation is crucial for addressing potential security threats and improving operational efficiency. As the industry continues to embrace innovation, eClinicalWorks remains at the forefront, empowering medical facilities to fully harness the capabilities of advanced analytics in their billing operations.
Allscripts: Integrated Revenue Cycle Management Solutions with EHR Systems
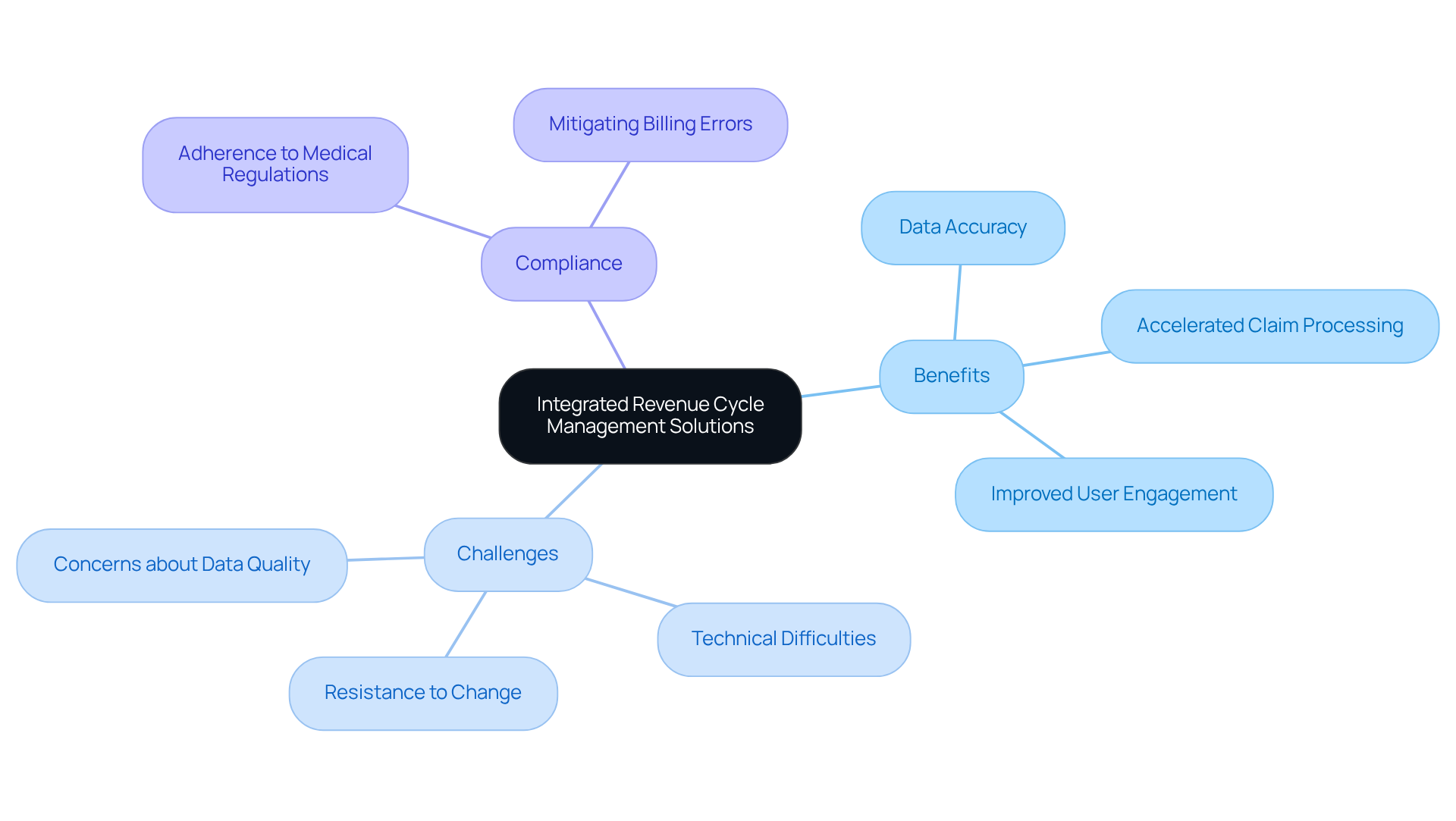
Allscripts offers integrated financial cycle management solutions that seamlessly connect with EHR systems, providing healthcare providers with a comprehensive approach to managing their financial operations. This integration enhances data accuracy, accelerates claim processing, and improves user engagement. By leveraging Allscripts’ solutions, medical organizations can optimize their revenue cycles with the help of revenue cycle management software vendors while prioritizing patient care.
Nonetheless, implementing these automated processes presents challenges. Organizations frequently encounter:
- Resistance to change from staff
- Technical difficulties
- Concerns about data quality
Effectively addressing these challenges necessitates clear communication and ongoing IT support to facilitate a smooth transition.
Additionally, compliance and risk management are vital aspects of the automation process. Ensuring that new systems adhere to medical regulations mitigates risks associated with billing errors, which is essential for maintaining financial stability.
As illustrated by Geisinger Health System, the successful implementation of processes with revenue cycle management software vendors not only enhances efficiency but also cultivates a culture of continuous improvement. This adaptability is crucial for healthcare providers as they respond to evolving patient needs while maintaining high standards of care. Furthermore, the integration of EHR systems has been shown to increase job satisfaction among staff, as automation allows them to focus on more complex cases, ultimately boosting team morale and improving patient outcomes.
Optum360: Enhancing Patient Financial Engagement through Revenue Cycle Management
Optum360 is dedicated to enhancing financial engagement for individuals through its innovative revenue cycle management solutions. By emphasizing clear communication and transparency, Optum360 empowers medical providers to improve collections and minimize outstanding balances.
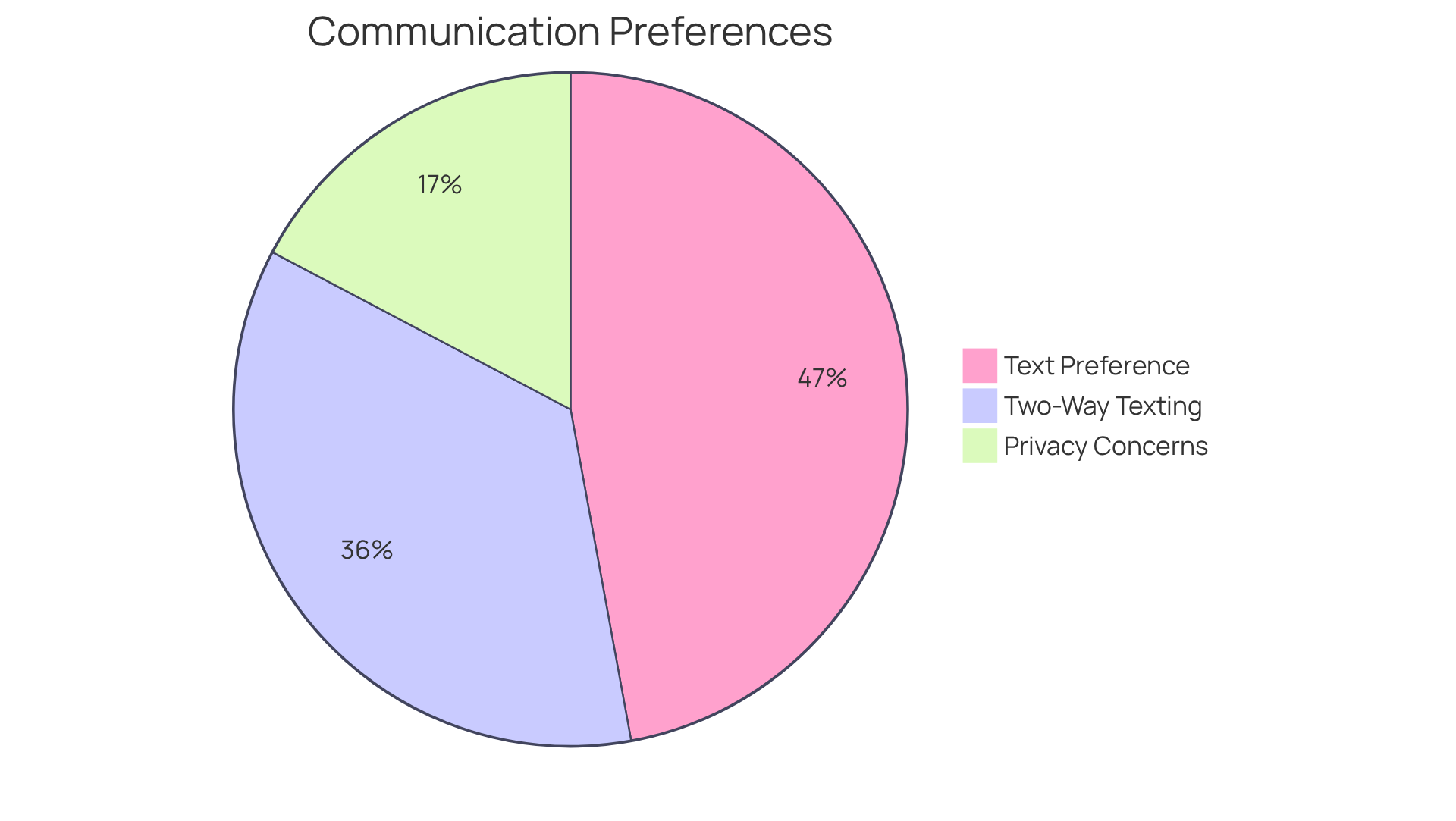
In 2026, effective communication with individuals is increasingly crucial, as 90% of people prefer to receive medical information via text. This trend underscores the need for medical organizations to actively involve individuals throughout their financial journey. Additionally, 68% of individuals prefer two-way texting with medical providers for inquiries or appointment rescheduling, highlighting the importance of interactive communication in boosting satisfaction and collections.
By ensuring that individuals are well-informed and engaged, Optum360 not only enhances satisfaction but also streamlines the overall financial process. However, it is essential to acknowledge that 33% of individuals cite privacy and security concerns as barriers to participating in medical texting.
As medical professionals adapt to evolving patient expectations, the impact of effective communication on collections becomes increasingly evident, establishing it as a vital component of successful income cycle management among revenue cycle management software vendors.
As noted by Sinch Engage:
- “The medical organizations that succeed in 2026 will be the ones that balance speed and convenience with trust, clarity, and responsiveness.
R1 RCM: End-to-End Revenue Cycle Management for Financial Optimization
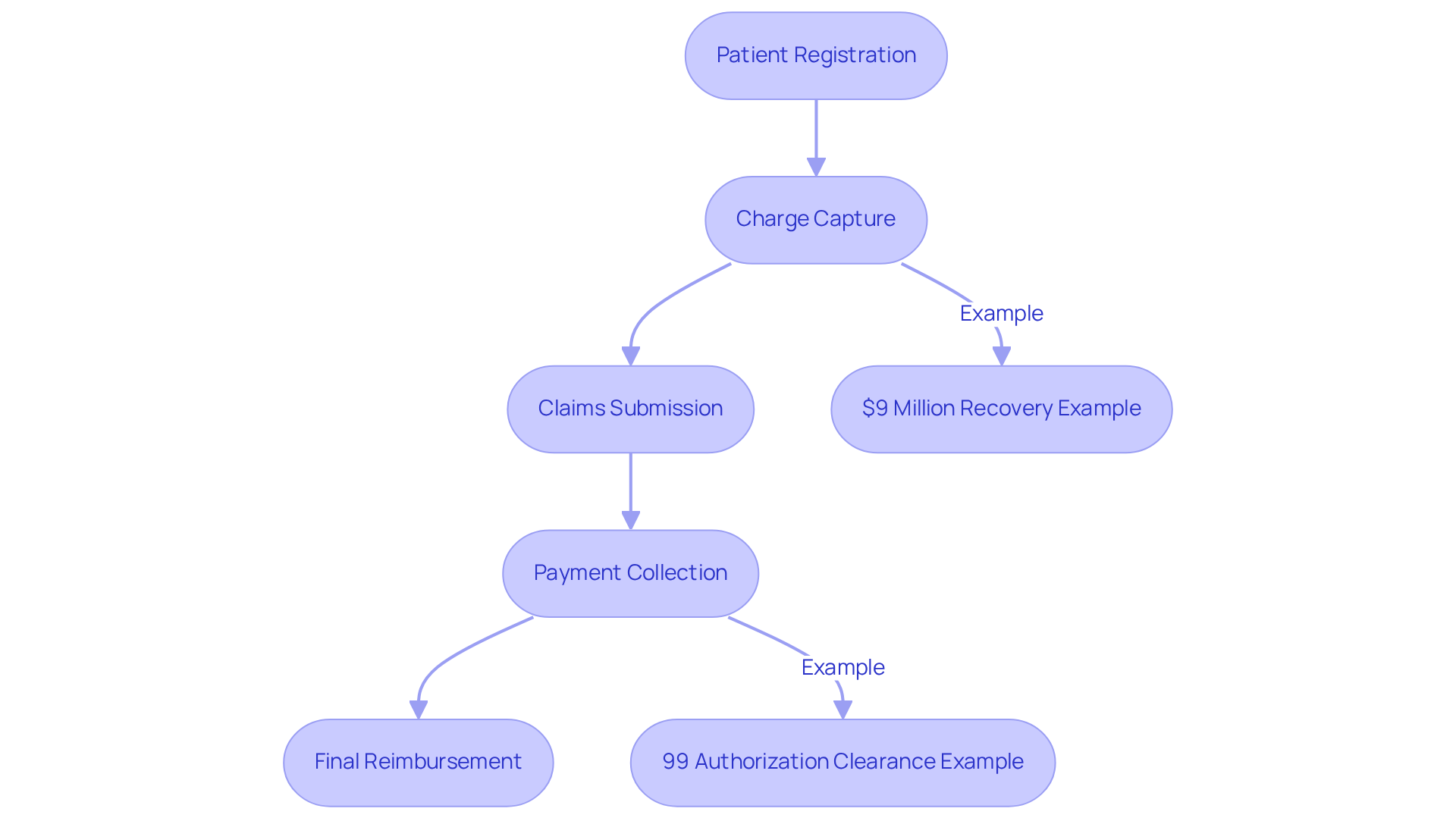
R1 RCM provides comprehensive end-to-end cycle management solutions that are tailored to enhance economic performance for healthcare organizations, as offered by revenue cycle management software vendors. Their approach encompasses every phase of the financial cycle, from patient registration to final payment collection, ensuring a seamless process that boosts operational efficiency. By utilizing advanced technology and analytics, R1 RCM enables providers to streamline operations, significantly reduce costs, and improve overall financial outcomes.
For example, a large Midwestern health system recovered $9 million in income within the first two years of implementing R1’s Charge Capture solution, illustrating the tangible benefits of their services. Additionally, R1’s innovative Phare Audit system, launched on January 8, aims to secure complete reimbursement and minimize income leakage, further establishing R1 RCM as a vital partner for medical organizations striving to enhance their financial cycles.
R1 has also been recognized as a 2026 ‘Best in KLAS’ award winner in multiple categories, highlighting their expertise and credibility in the industry. Furthermore, the success of Baptist Health Care in clearing 99% of authorizations within three days exemplifies the operational efficiency achieved through R1’s services. As the medical field continues to evolve, the integration of technology and data-driven insights remains essential for economic optimization, positioning R1 RCM as a leader among revenue cycle management software vendors in this critical sector.
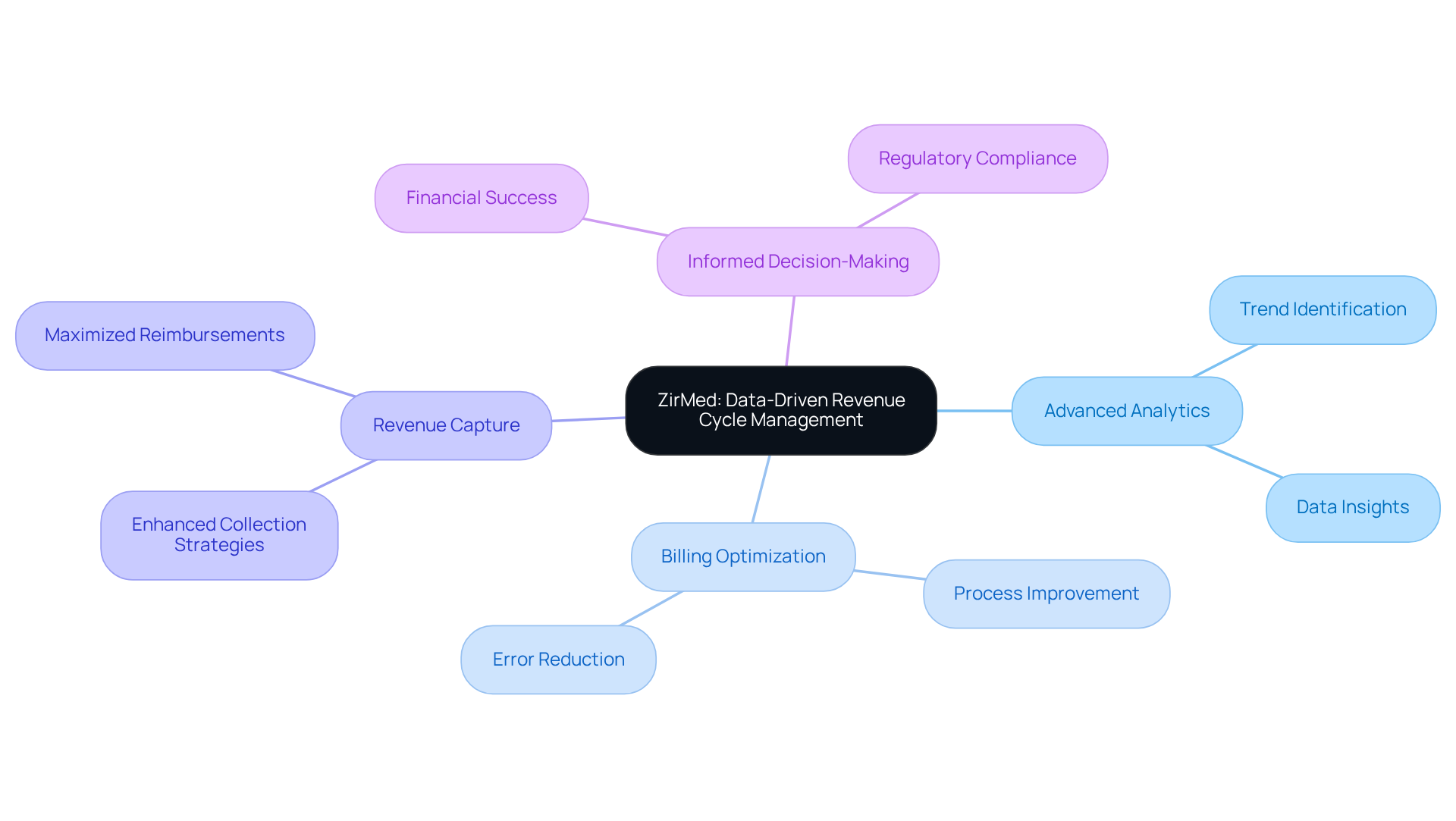
ZirMed: Data-Driven Revenue Cycle Management for Improved Financial Outcomes
ZirMed, now integrated with Waystar, offers solutions from revenue cycle management software vendors that are data-driven and designed to improve economic outcomes for medical providers. Their platform employs advanced analytics to identify trends, optimize billing processes, and enhance overall revenue capture through revenue cycle management software vendors. By leveraging data insights, ZirMed enables healthcare organizations to make informed decisions that promote financial success and ensure compliance with industry regulations.
Conclusion
In navigating the landscape of revenue cycle management (RCM), selecting the right software vendor is crucial for optimizing financial performance in healthcare organizations. This article highlights ten notable vendors, each offering unique solutions tailored to address the specific challenges faced by medical providers. By understanding the capabilities and innovations of these vendors, healthcare organizations can enhance their operational efficiency and improve their financial outcomes.
Key insights from the article reveal that vendors like Neutech and NextGen Healthcare focus on tailored solutions and integrated systems, respectively, to minimize claim denials and streamline billing processes. Athenahealth’s cloud-based platform showcases the importance of real-time data access, while Cerner emphasizes automation to enhance cash flow. Similarly, McKesson and eClinicalWorks provide cost-effective and innovative solutions that leverage advanced analytics and automation to boost billing efficiency. The article also underscores the significance of patient engagement, as demonstrated by Optum360, and the comprehensive approach of R1 RCM in managing the entire revenue cycle.
Ultimately, as the healthcare industry continues to evolve, the integration of advanced technologies and data-driven insights will be paramount for organizations seeking to thrive financially. Embracing these revenue cycle management solutions not only addresses immediate financial challenges but also positions healthcare providers for long-term success in a competitive landscape. Engaging with the right RCM software vendors can lead to improved patient care and economic sustainability, making it essential for healthcare organizations to carefully evaluate their options and invest in solutions that align with their goals.
Frequently Asked Questions
What is Neutech’s approach to revenue cycle management (RCM) solutions?
Neutech offers tailored RCM solutions that address the unique challenges of regulated industries, focusing on compliance and operational efficiency to help medical providers navigate the complex billing and coding landscape.
How does Neutech ensure the quality of its services?
Neutech has a high employee retention rate, ensuring clients benefit from a stable and knowledgeable team. Additionally, their zero-bench philosophy keeps all engineers actively engaged, promoting consistent quality and seamless scalability.
What impact can Neutech’s solutions have on claim denial rates?
Neutech’s customized systems can reduce claim denial rates by as much as 75%, significantly improving the financial health of medical organizations.
How does Neutech engage with its clients?
Neutech’s client engagement process includes personalized consultations and careful selection of specialized developers and designers to meet the unique needs of each medical provider.
What is NextGen Healthcare’s role in revenue cycle management?
NextGen Healthcare provides an integrated solution for RCM and electronic health records (EHR), enhancing billing processes and financial performance for medical practitioners by minimizing errors and accelerating collections.
What market position does NextGen Healthcare hold?
As of 2026, NextGen Healthcare is a market leader in financial cycle management, reflecting its commitment to innovation and efficiency in medical services.
What results have providers seen from using NextGen’s RCM solutions?
Providers using NextGen’s RCM solutions have reported improvements in cash flow and decreased denial rates, showcasing the effectiveness of their integrated approach.
How does Athenahealth enhance billing efficiency for medical providers?
Athenahealth provides a cloud-based financial cycle management solution that allows real-time access to billing data, facilitating faster claim submissions and improved reimbursement tracking.
What innovations has Athenahealth introduced to improve RCM?
In 2025, Athenahealth introduced AI-enabled features that resulted in a 36% reduction in insurance-related claim holds, saving over 6,500 hours in administrative time.
What are the expected outcomes of Athenahealth’s innovations?
Athenahealth aims to reduce at least 50% of the current financial cycle management workload over the next three years, transforming how providers manage their billing processes.
How does Athenahealth’s cloud technology benefit healthcare providers?
The integration of cloud technology accelerates reimbursements and helps medical organizations navigate evolving health policies, enhancing overall billing efficiency.
What specific feature helps decrease patient insurance-related denials with Athenahealth’s solutions?
The automated insurance selection feature decreases patient insurance-related denials by 13%, demonstrating the effectiveness of Athenahealth’s solutions in improving billing efficiency.