4 Best Practices for Software Development in Medical Applications

Introduction
The intersection of technology and healthcare is rapidly evolving, presenting both opportunities and challenges for software developers. As the demand for innovative medical applications increases, understanding best practices is crucial for ensuring compliance and enhancing patient care. Developers must navigate the complex landscape of regulations while leveraging emerging technologies to create effective solutions. This article explores essential strategies for software development in medical applications, highlighting key practices that can lead to successful outcomes in an increasingly regulated environment.
Understand Regulatory Requirements in Healthcare Software Development
In the healthcare sector, software development medical professionals face a complex landscape of regulations governing data privacy, security, and patient safety. Key regulations include the Health Insurance Portability and Accountability Act (HIPAA), which mandates the protection of patient information, and the Food and Drug Administration (FDA) guidelines for software classified as a medical device (SaMD). The U.S. Department of Health and Human Services reported over 22 enforcement actions in 2022, primarily targeting HIPAA Right of Access violations, underscoring the critical need for compliance.
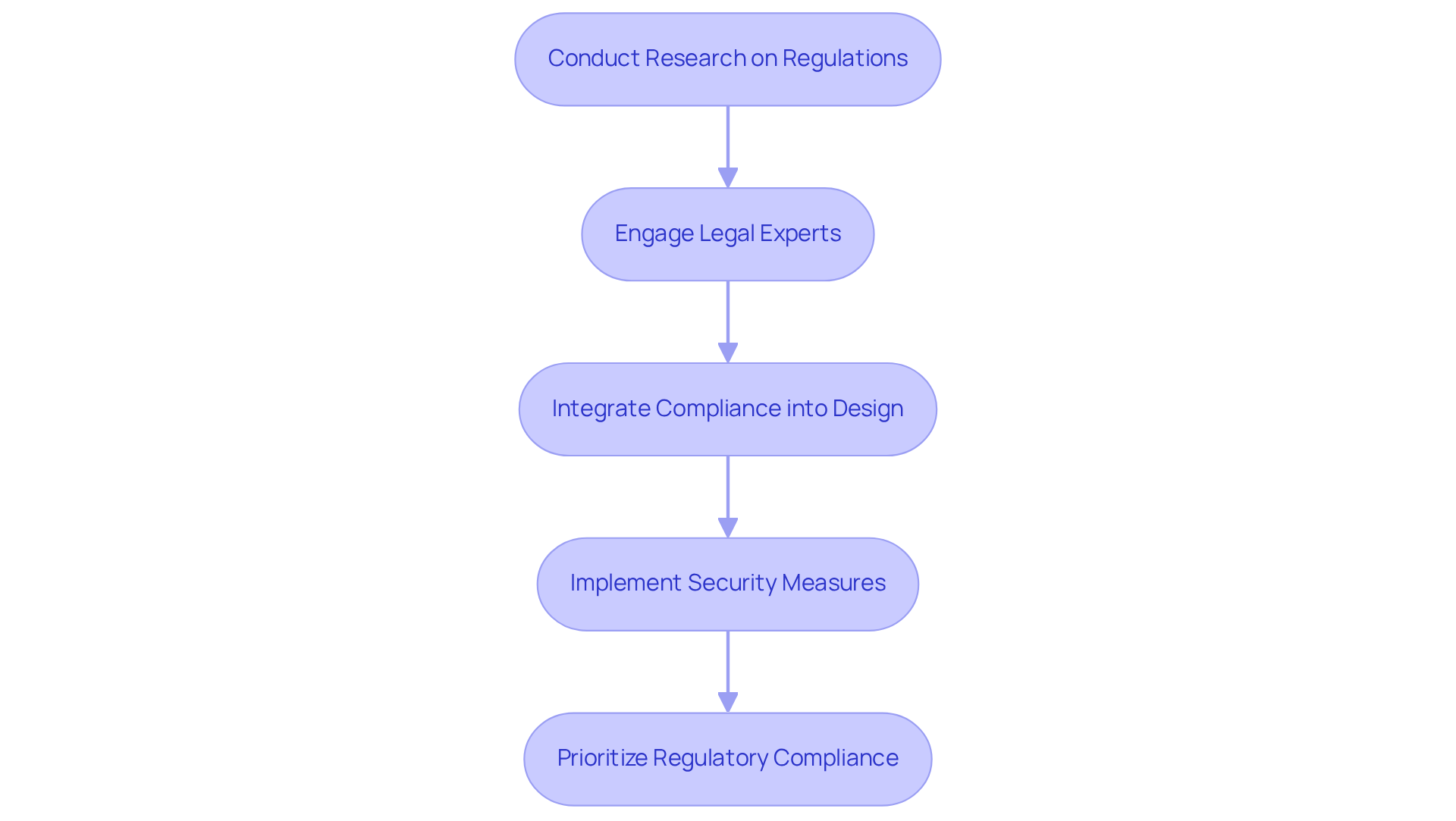
To ensure compliance, developers should take several key steps:
- Conduct thorough research on applicable regulations early in the development process. This foundational step is crucial, as the compliance landscape is continually evolving, with significant updates anticipated in 2025 and 2026 that will influence software development in the medical sector.
- Engage legal and compliance experts to interpret regulations and integrate them into the software design. As Holly Little, a healthcare and life sciences attorney, notes, ‘Integrating compliance into the software development medical lifecycle is not just a legal obligation but a critical component of delivering safe and effective healthcare solutions.’
- Implement security measures such as encryption and access controls to safeguard sensitive data. The enforcement landscape is shifting, with regulators increasingly scrutinizing operational failures that result in data breaches.
By prioritizing regulatory compliance, developers in software development medical can mitigate risks and enhance the trustworthiness of their applications, ultimately leading to improved patient outcomes and reduced liability for healthcare providers. Successful software development medical projects in healthcare, such as those developed by Neutech, illustrate the effectiveness of adhering to HIPAA and FDA regulations, demonstrating how compliance can drive innovation while ensuring patient safety.
Identify Key Types of Healthcare Software Solutions
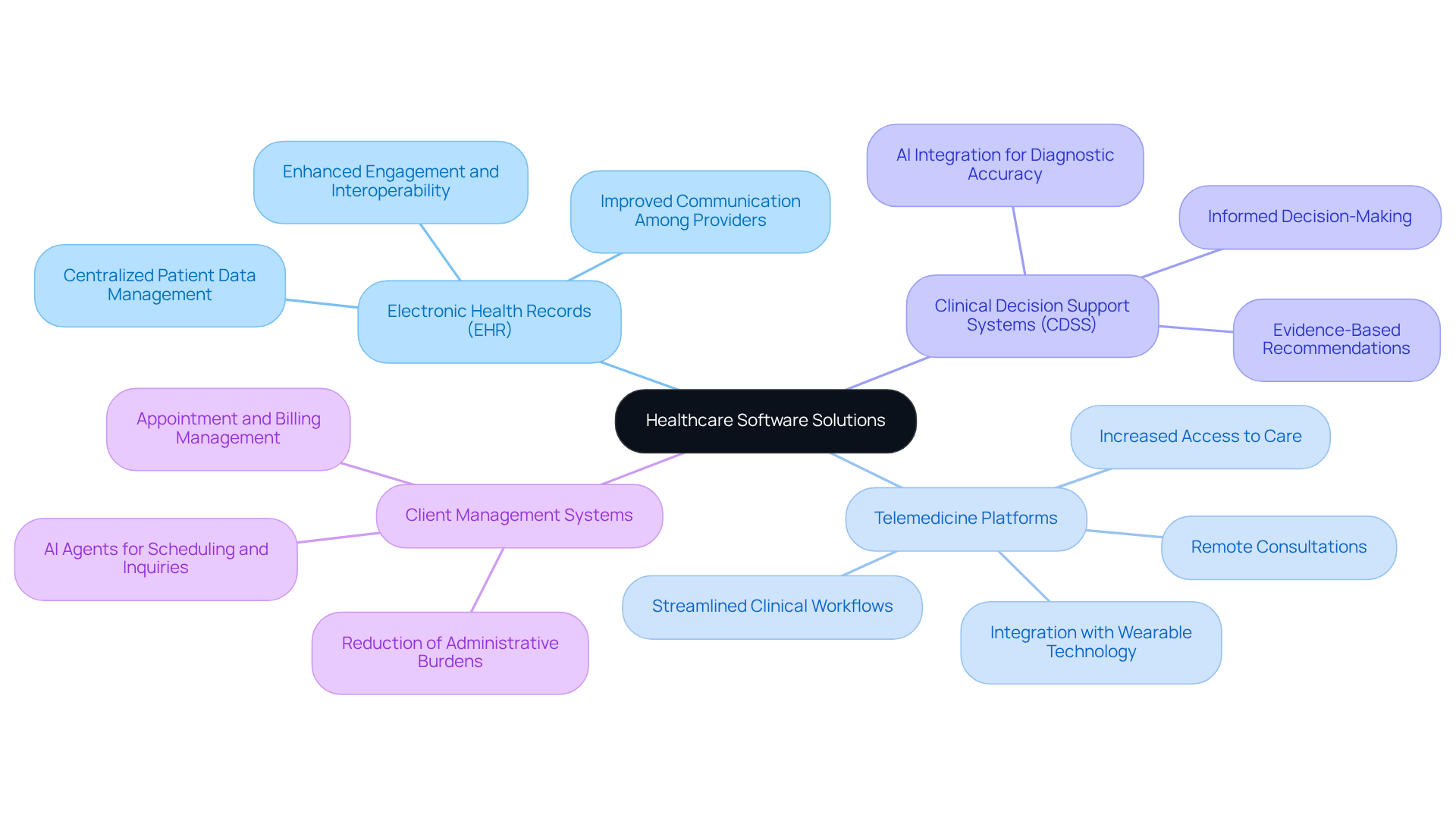
The field of software development medical encompasses a wide array of applications aimed at enhancing care and streamlining operational workflows. The primary categories include:
-
Electronic Health Records (EHR): Centralized systems that manage patient data, EHRs foster improved communication among healthcare providers and ensure continuity of care. Their integration is crucial, as it promotes interoperability and enhances engagement by providing easier access to health records.
-
Telemedicine Platforms: These innovative solutions enable remote consultations, significantly broadening access to care, particularly in underserved areas. The growth of telemedicine is noteworthy; a recent study indicates that 76% of hospitals in the U.S. now facilitate remote connections between doctors and patients, a substantial increase from 35% a decade ago. Furthermore, 40% of Americans utilize wearable technology for health monitoring, which complements telemedicine by allowing continuous tracking of health metrics. This transition not only enhances convenience for individuals but also simplifies clinical workflows, reducing unnecessary hospital visits.
-
Clinical Decision Support Systems (CDSS): These tools empower healthcare professionals by offering evidence-based recommendations derived from individual patient data and clinical guidelines. The incorporation of AI within CDSS enhances diagnostic accuracy and aids clinicians in making informed decisions, ultimately leading to improved health outcomes.
-
Client Management Systems: This software aids in managing client appointments, billing, and follow-ups, thereby reducing administrative burdens and enhancing operational efficiency. By automating routine tasks, these systems allow medical providers to focus more on patient care rather than administrative duties. Additionally, AI agents can handle appointment scheduling and patient inquiries, mitigating physician burnout and improving overall efficiency.
By concentrating on these critical areas, professionals can utilize software development medical to develop tailored solutions that effectively address the unique challenges within the medical sector, resulting in better patient outcomes and increased operational efficiency. The landscape of software development medical in 2026 is characterized by rapid growth and heightened regulation, underscoring the importance for developers to remain informed and adaptable.
Implement a Structured Software Development Life Cycle (SDLC)
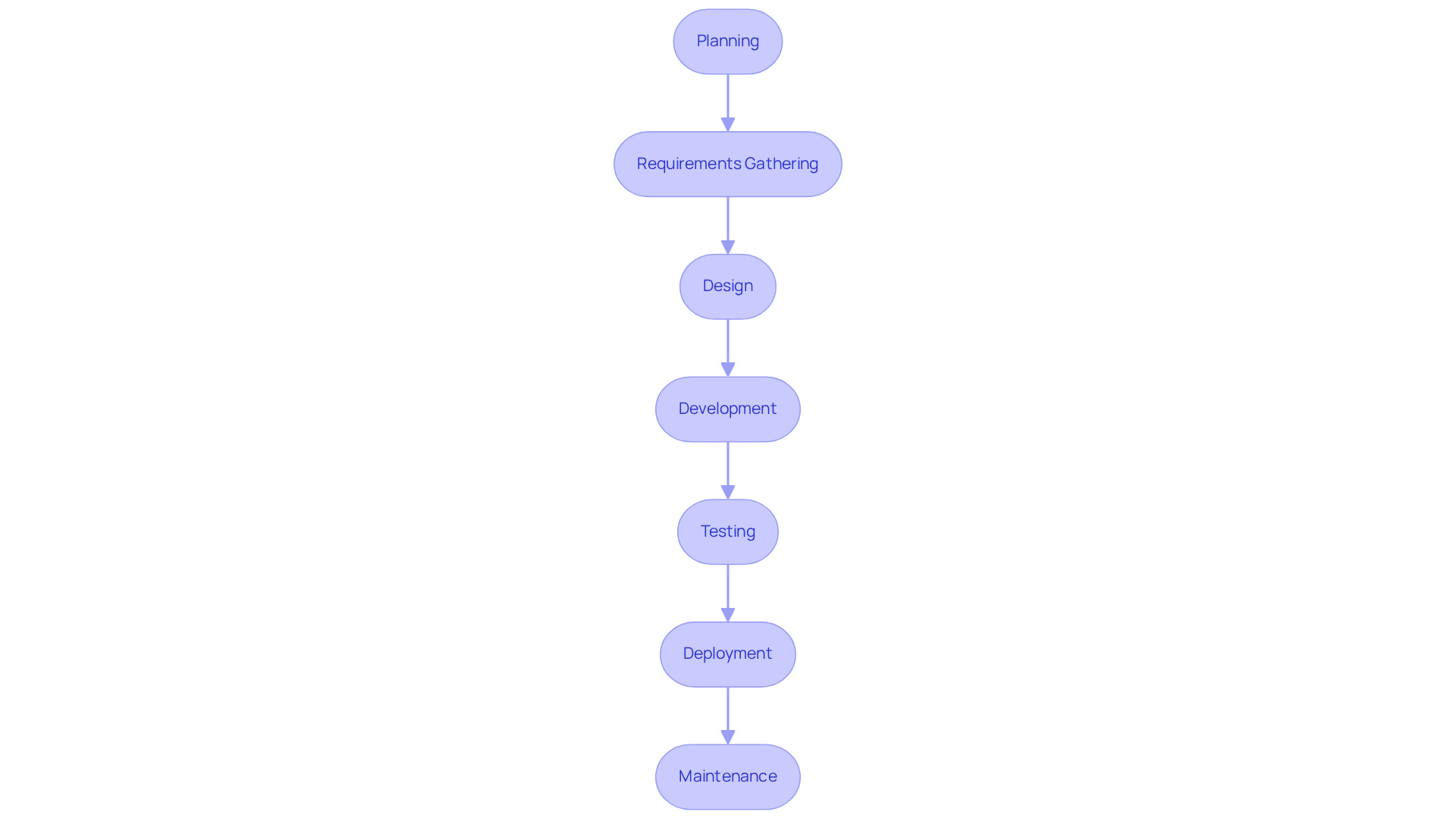
A well-defined software development medical life cycle (SDLC) is essential for the development of healthcare applications. This process typically encompasses several key phases:
- Planning: This phase involves defining the project scope, objectives, and the resources required for successful execution.
- Requirements Gathering: Collaboration with stakeholders is crucial to gather and document both functional and non-functional requirements.
- Design: During this phase, architectural designs are created to ensure alignment with regulatory standards and user needs.
- Development: Coding practices are implemented with a strong emphasis on security and compliance to safeguard sensitive information.
- Testing: Rigorous testing is conducted, including unit, integration, and user acceptance testing, to verify that the application meets established quality standards.
- Deployment: The application is rolled out in a controlled manner, ensuring that all stakeholders receive adequate training.
- Maintenance: A comprehensive plan is established for ongoing support and updates, addressing any issues that arise and adapting to evolving regulations.
By adhering to a structured SDLC, developers can significantly enhance the reliability and safety of their applications in software development medical, ultimately leading to improved care for individuals.
Leverage Emerging Technologies for Enhanced Software Quality
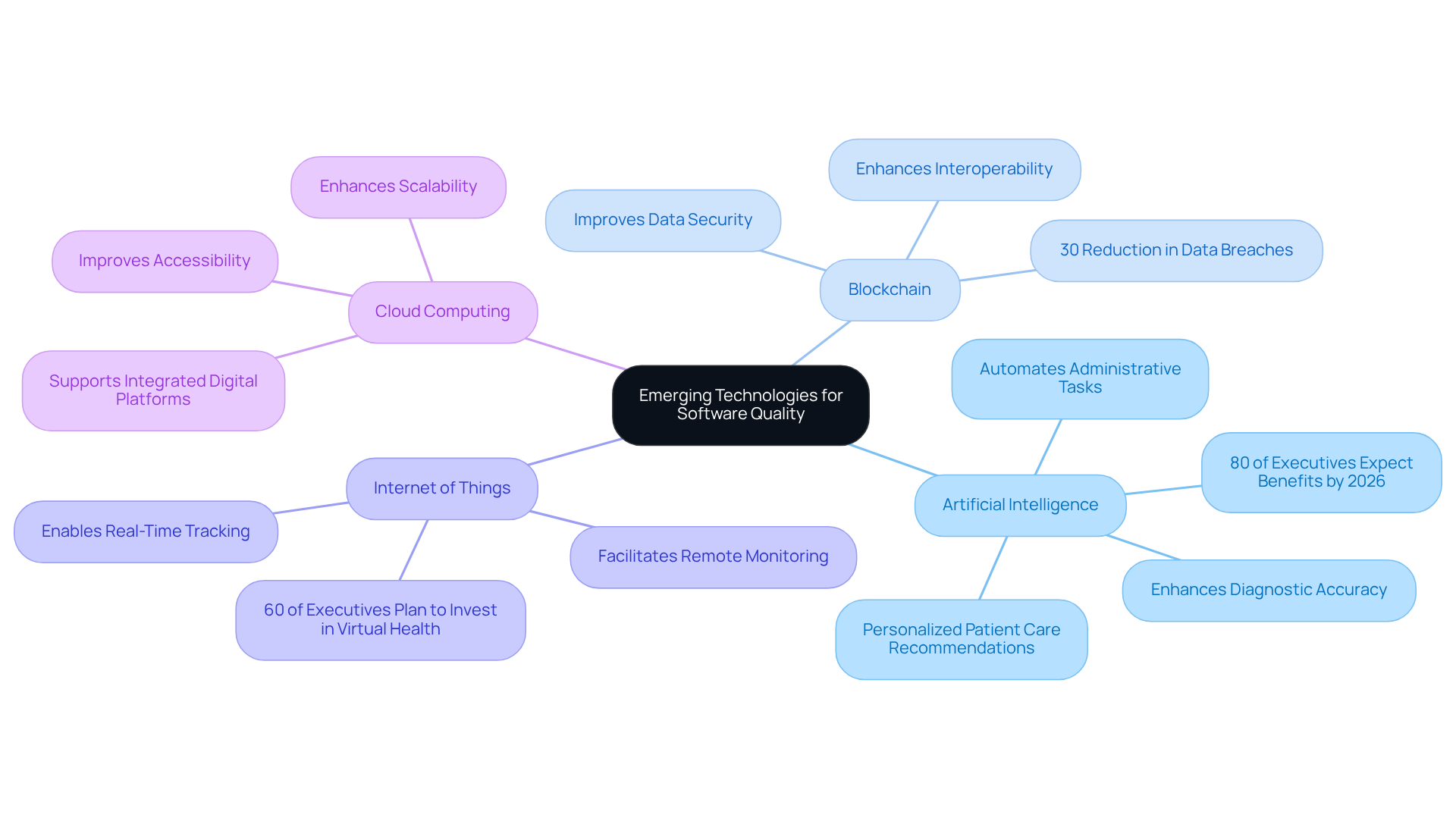
Integrating emerging technologies into software development medical can result in significant improvements in quality and user experience. Key technologies to consider include:
-
Artificial Intelligence (AI): AI enhances diagnostic accuracy, automates administrative tasks, and provides personalized patient care recommendations. With over 80% of health system executives anticipating that generative AI will deliver substantial benefits across clinical functions by 2026, its integration is becoming essential for modern medical services.
-
Blockchain: This technology improves data security and interoperability by offering a decentralized and tamper-proof record of individual information. Successful implementations have shown that blockchain can significantly reduce data breaches, which have increased in recent years, making it a vital component for compliance with regulations such as HIPAA. For example, a recent study indicated that organizations utilizing blockchain technology experienced a 30% reduction in data breach incidents.
-
Internet of Things (IoT): IoT devices facilitate remote monitoring of individuals, enabling medical professionals to track well-being in real-time. Nearly 60% of health plan executives intend to invest in virtual health services, which frequently depend on IoT technology to improve preventive care.
-
Cloud Computing: Leveraging cloud services enhances scalability and accessibility, allowing providers to access data from any location. This flexibility is crucial as healthcare organizations increasingly adopt integrated digital platforms to streamline operations and improve outcomes.
By harnessing these technologies, software development medical developers can create innovative solutions that not only comply with regulatory requirements but also significantly enhance patient outcomes and operational efficiency.
Conclusion
Prioritizing best practices in software development for medical applications is crucial for ensuring compliance, enhancing patient care, and streamlining operational efficiency. By comprehending the regulatory landscape, developers can create solutions that not only meet legal standards but also build trust among healthcare providers and patients.
This article highlights four key practices:
- Understanding regulatory requirements
- Identifying essential software solutions
- Implementing a structured software development life cycle (SDLC)
- Leveraging emerging technologies
Each of these components is vital in the development process, ensuring applications adhere to HIPAA and FDA guidelines while utilizing AI and blockchain for improved data security and patient outcomes.
As the healthcare software landscape evolves, the significance of these practices is paramount. Developers must remain adaptable and informed about forthcoming regulations and technologies that will shape the industry in the years ahead. Embracing these best practices will enhance the quality of healthcare software and contribute to a more efficient, patient-centered healthcare system.
Frequently Asked Questions
What are the main regulatory requirements for healthcare software development?
Key regulatory requirements include the Health Insurance Portability and Accountability Act (HIPAA), which mandates the protection of patient information, and the Food and Drug Administration (FDA) guidelines for software classified as a medical device (SaMD).
Why is compliance with regulations important in healthcare software development?
Compliance is critical to protect patient information, ensure patient safety, and mitigate risks associated with data breaches and operational failures. It also enhances the trustworthiness of applications and can lead to improved patient outcomes.
What recent enforcement actions have been reported related to healthcare software compliance?
The U.S. Department of Health and Human Services reported over 22 enforcement actions in 2022, primarily targeting HIPAA Right of Access violations, highlighting the importance of compliance.
What steps should developers take to ensure compliance with healthcare regulations?
Developers should conduct thorough research on applicable regulations early in the development process, engage legal and compliance experts to interpret regulations, and implement security measures such as encryption and access controls.
How can integrating compliance into the software development lifecycle benefit healthcare solutions?
Integrating compliance is not only a legal obligation but also a critical component of delivering safe and effective healthcare solutions, ultimately enhancing patient safety and reducing liability for healthcare providers.
Can you provide an example of successful healthcare software development that adheres to regulations?
Successful projects, such as those developed by Neutech, demonstrate the effectiveness of adhering to HIPAA and FDA regulations, showing that compliance can drive innovation while ensuring patient safety.