Comparing Medical Software Used in Hospitals: Features and Benefits

Introduction
In the rapidly evolving landscape of healthcare, advanced medical software has become essential for hospitals aiming to improve patient care and operational efficiency. This article explores the different types of medical software used in hospital environments, emphasizing their distinct features and the significant advantages they provide.
As hospitals increasingly embrace these technologies, they encounter critical challenges:
- How can they effectively manage the complexities of implementation?
- What key factors must they consider to ensure these systems adequately address their diverse needs?
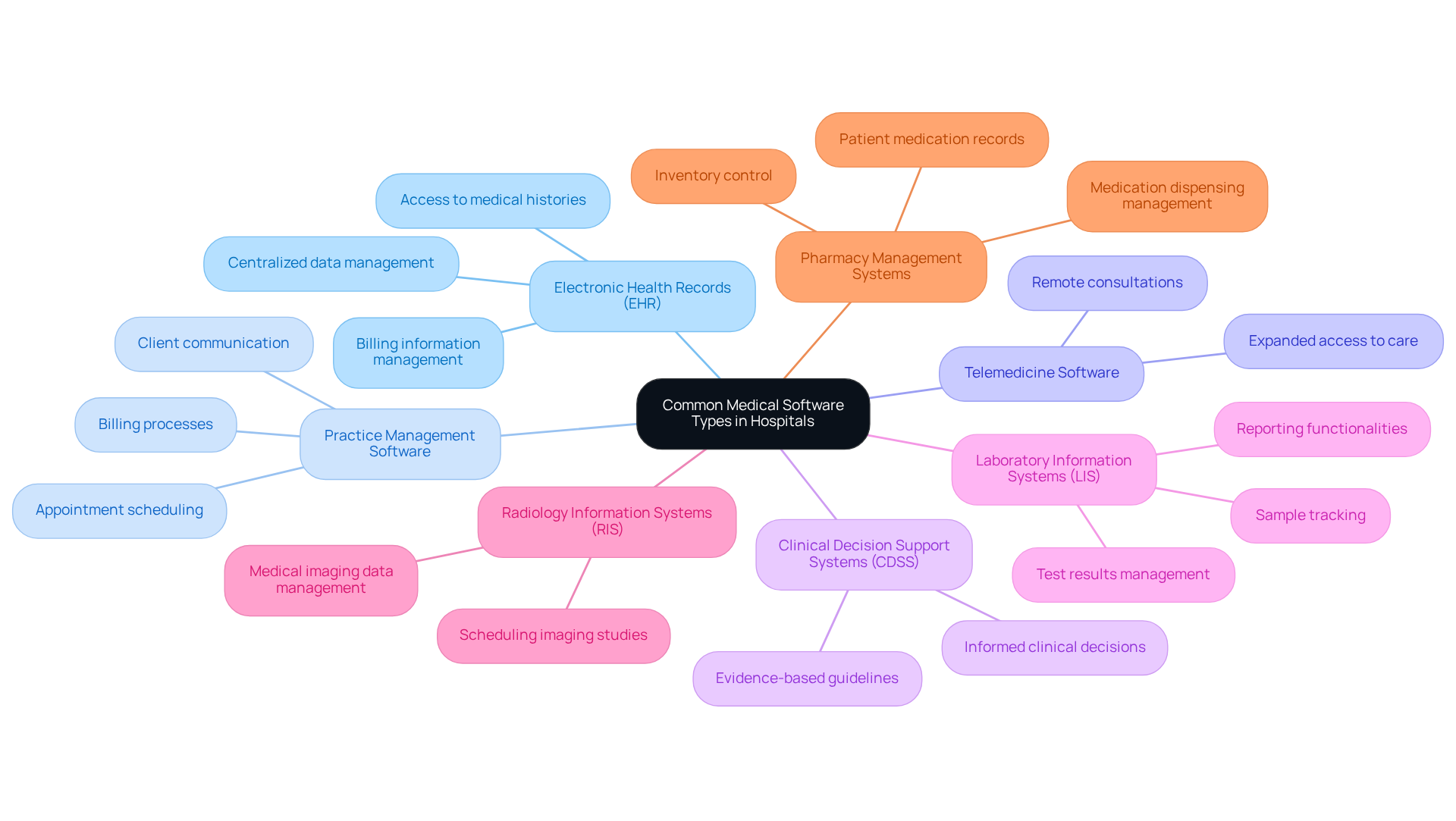
Overview of Common Medical Software Types in Hospitals
In hospitals, medical software used in hospitals is employed to improve operational efficiency and patient care. The key categories include:
- Electronic Health Records (EHR): These centralized systems manage individual data, allowing for easy access to medical histories, treatment plans, and billing information.
- Practice Management Software: This category encompasses tools that streamline administrative tasks, such as appointment scheduling, billing, and client communication.
- Telemedicine Software: These platforms facilitate remote consultations between medical providers and patients, which is essential for expanding access to care.
- Clinical Decision Support Systems (CDSS): This software aids healthcare professionals in making informed clinical decisions based on individual data and evidence-based guidelines.
- Laboratory Information Systems (LIS): These systems manage laboratory operations, including sample tracking, test results, and reporting.
- Radiology Information Systems (RIS): Designed to manage medical imaging data, this software includes functionalities for scheduling, tracking, and reporting imaging studies.
- Pharmacy Management Systems: These tools assist in managing medication dispensing, inventory, and medication records for patients.
Together, these application categories significantly enhance health outcomes and operational efficiencies within hospital environments through medical software used in hospitals.
Key Features of Top Medical Software Solutions
When evaluating medical software solutions, several key features emerge as essential for effective healthcare delivery:
-
Interoperability: Smooth data transfer among various systems is crucial for integrated care. It allows medical providers to access complete patient information and coordinate treatment efficiently. The global medical interoperability solutions market was valued at $2.9 billion in 2021 and is projected to reach $5.7 billion by 2026, underscoring the growing importance of these solutions.
-
User-Friendly Interface: An intuitive design minimizes training time and enhances user adoption. This ensures that medical professionals can quickly adapt to the application without extensive learning curves.
-
Data Security: Strong security measures, including encryption and access controls, are vital for safeguarding sensitive patient information and preserving trust in medical systems.
-
Customization: The ability to tailor applications to specific hospital workflows and requirements allows for greater flexibility and efficiency in operations.
-
Analytics and Reporting: Advanced tools for data analysis support clinical decision-making and operational improvements. They aid medical providers in deriving actionable insights from their data. However, it is important to note that only 57% of practices using AI tools report a positive return on investment, indicating the need for careful implementation of AI in medical software.
-
Mobile Access: Remote access through mobile devices enhances care delivery on-the-go. This ensures that providers can respond to individuals’ needs promptly, regardless of their location.
-
Compliance Features: Built-in functionalities that ensure adherence to medical regulations and standards, such as HIPAA, are essential for maintaining legal compliance and protecting individual data.
As Colleen Sirhal, Chief Clinical Officer at Hyland, stated, “The significance of interoperability in the medical field has been evident for a while – and it is only increasing in significance.” These features of medical software used in hospitals are not merely beneficial but essential for enhancing operational efficiency and improving patient care outcomes. As medical services continue to advance, the significance of interoperability in clinical applications will only increase, with specialists highlighting its role in achieving connected care and efficient operations.

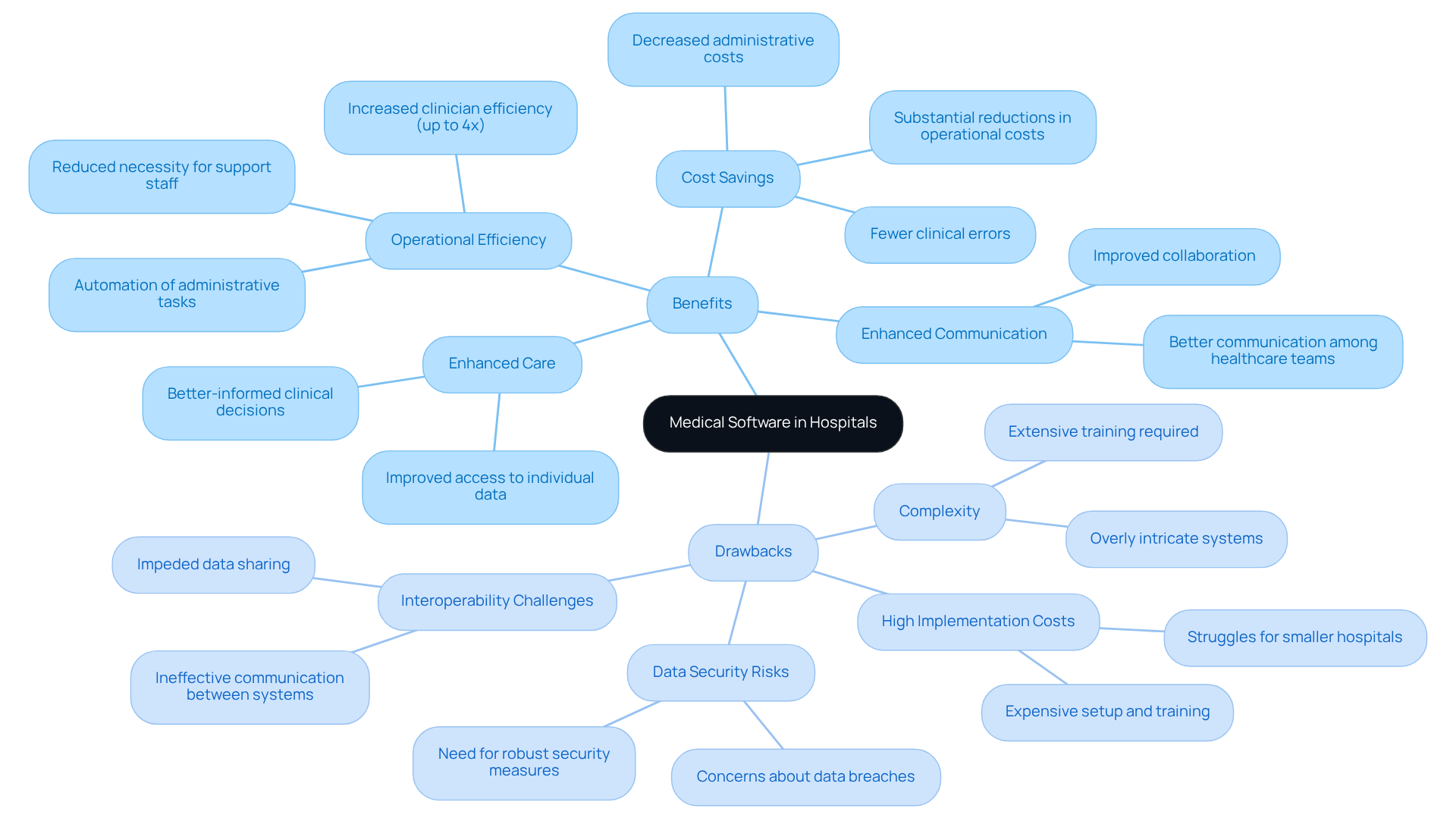
Benefits and Drawbacks of Medical Software in Hospital Settings
The advantages offered by medical software used in hospitals can significantly enhance operations.
-
Enhanced Care: Improved access to individual data enables medical professionals to make better-informed clinical decisions, ultimately leading to improved outcomes for patients.
-
Operational Efficiency: The automation of administrative tasks not only reduces workload but also minimizes errors, allowing healthcare staff to concentrate more on patient care. Experts indicate that the use of medical software used in hospitals can increase clinician efficiency by up to four times, thereby reducing the necessity for extensive support staff. Additionally, 67% of U.S. physicians plan to increase their expenditure on medical software used in hospitals in the coming year, reflecting a growing commitment to tools that enhance operational efficiency.
-
Cost Savings: Streamlined processes can result in substantial reductions in operational costs over time. While the initial investment in medical software used in hospitals may be significant, long-term savings include decreased administrative costs and fewer clinical errors, making the investment worthwhile. Automation can notably lower medical costs by enhancing clinician efficiency.
-
Enhanced Communication: Effective medical applications promote better communication among healthcare teams, improving collaboration and ensuring continuity of care.
Despite these advantages, hospitals must also consider notable drawbacks:
-
High Implementation Costs: The initial setup and training for new systems can be prohibitively expensive, particularly for smaller hospitals that may struggle to absorb these costs.
-
Complexity: Some systems can be overly intricate, requiring extensive training and adjustment periods that can disrupt existing workflows.
-
Data Security Risks: Increased reliance on digital systems raises significant concerns regarding data breaches and cyber threats, necessitating robust security measures.
-
Interoperability Challenges: Not all systems communicate effectively, which can impede data sharing and integrated care, complicating the delivery of comprehensive patient services.
Healthcare leaders emphasize the importance of strategic budgeting and thorough assessment of medical software used in hospitals to effectively address these challenges. As one expert noted, “Success in the medical field will depend on informed technology decisions that prioritize measurable value and security.” This underscores the necessity for hospitals to weigh both the potential benefits and inherent risks when selecting medical technology solutions. Furthermore, as healthcare practices anticipate significant financial shifts in 2026, including rising software costs and workforce strain, it is crucial for decision-makers to stay informed about the evolving landscape.
Suitability of Medical Software for Diverse Hospital Needs
Hospitals have distinct needs that vary according to their size, specialty, and patient demographics. To effectively assess the suitability of medical software, consider the following factors:
- Size of the Hospital: Larger hospitals typically require comprehensive systems that integrate multiple functionalities. In contrast, smaller facilities may find greater value in simpler, more focused solutions.
- Specialty Services: Hospitals that concentrate on specific fields, such as pediatrics or oncology, often need tools tailored to their unique clinical workflows and regulatory requirements.
- Client Volume: Facilities with high patient volumes necessitate robust systems capable of managing large datasets and providing quick access to information.
- Budget Constraints: Financial considerations are crucial; hospitals must weigh the cost of technology against the anticipated return on investment.
- Regulatory Compliance: It is essential that solutions adhere to industry standards and regulations, particularly concerning data security and patient privacy.
By thoroughly evaluating these factors, hospitals can select medical software that aligns with their operational needs and enhances the quality of patient care.

Conclusion
The exploration of medical software utilized in hospitals underscores its critical role in enhancing patient care and operational efficiency. By integrating systems such as Electronic Health Records and Clinical Decision Support Systems, hospitals can streamline processes, improve communication, and ultimately achieve better healthcare outcomes.
Key insights reveal essential features of effective medical software, including:
- Interoperability
- User-friendly interfaces
- Robust data security measures
While the advantages of improved care access and operational cost savings are substantial, it is vital to recognize the challenges, such as:
- High implementation costs
- Potential data security risks
Hospitals must meticulously assess their specific needs and constraints to select the most appropriate software solutions.
In an ever-evolving healthcare landscape, the significance of informed technology choices cannot be overstated. Decision-makers should prioritize systems that not only address current operational demands but also adapt to future challenges. By doing so, hospitals can ensure they remain at the forefront of delivering quality patient care while effectively navigating the complexities of modern medical software.
Frequently Asked Questions
What is the purpose of medical software in hospitals?
Medical software in hospitals is used to improve operational efficiency and patient care.
What are Electronic Health Records (EHR)?
EHR are centralized systems that manage individual patient data, allowing easy access to medical histories, treatment plans, and billing information.
What does Practice Management Software do?
Practice Management Software encompasses tools that streamline administrative tasks such as appointment scheduling, billing, and client communication.
How does Telemedicine Software benefit patients?
Telemedicine Software facilitates remote consultations between medical providers and patients, expanding access to care.
What is the role of Clinical Decision Support Systems (CDSS)?
CDSS aids healthcare professionals in making informed clinical decisions based on individual patient data and evidence-based guidelines.
What functions do Laboratory Information Systems (LIS) provide?
LIS manage laboratory operations, including sample tracking, test results, and reporting.
What is the purpose of Radiology Information Systems (RIS)?
RIS is designed to manage medical imaging data, including functionalities for scheduling, tracking, and reporting imaging studies.
How do Pharmacy Management Systems assist hospitals?
Pharmacy Management Systems assist in managing medication dispensing, inventory, and medication records for patients.
What overall impact do these medical software categories have in hospitals?
Together, these application categories significantly enhance health outcomes and operational efficiencies within hospital environments.